Whilst there had been occasional ductal ligations performed at Wellington Hospital (8 patients operated on between 1944 and 1952), a focus on congenital heart disease in Wellington and in other NZ centres began after Green Lane Hospital pioneered palliation or correction of selected congenital cardiac defects.
The surgeons at Green Lane Hospital were the first in NZ to carry out a Blalock anastomosis for Tetralogy of Fallot (1948), pulmonary valvotomy (1953), and atrial septal defect closure (1954).
Thus began in Wellington the investigation by cardiac catheterisation of both children and adults with suspected congenital heart disease. The fact that there had been no treatment previously available was the reason for a significant number of older patients in this group. Quite quickly, a pool of patients built up and referrals of some to Green Lane Hospital began. Between 1954 and 1958, between one and four patients were referred annually.
The first referral to Green Lane Hospital occurred in 1954.
This was a cyanosed 25yr old man, L.M., who had undergone cardiac catheterisation in 1952. The operator was Verney Cable who was assisted by Marshall Luke (medical registrar). This was just the third cardiac catheter done at Wellington Hospital. Marshall Luke recalls well Verney's delight when the catheter passed directly from RV to ascending aorta. A diagnosis of Tetralogy of Fallot was made.
The patient was referred to Green Lane Hospital where Rowan Nicks created a (L) Blalock shunt. The result was very successful with markedly reduced cyanosis and the patient was relatively well for the next 16 years.
By that time he was on the staff of Wellington Hospital as a biomedical technician and he approached Ron Easthope to ask if anything more could be done, as by now he had some limitation of effort capacity.
Ron undertook cardiac catheterisation on 30/7/1970, demonstrating a patent but narrowed Blalock anastomosis, severe RV outflow obstruction and significant R to L shunting. |
The patient was accepted for surgical correction at Wellington Hospital
15/4/1971, Correction of Tetralogy of Fallot and ligation of Blalock shunt.
Surgeon Jim Baird
Operation began at 0840hrs and ended at 1615hrs!
Total bypass time 121 minutes. |
The numbers of children with congenital heart disease undergoing cardiac catheterisation at Wellington Hospital steadily increased from 16 in 1955 to 62 in 1964. There was a sharp increase in referrals to Green Lane in 1959 (15 patients), and seven in 1960, but thereafter the numbers declined as James Baird and Tim Savage were gearing up to carry out surgery for congenital heart disease in Wellington.
A major part of the preparations for this type of surgery was a series of animal surgical procedures. From November 1961 to July 1963, 36 dog procedures were undertaken, each testing a variety of aspects of hypothermic cardiac surgery.
Tim Savage's recollections
A 'waiting list' of patients with secundum ASD was allowed to develop, so that the surgeons were able to carry out ASD closure on seven patients in each of the two years 1962 and 1963. These procedures were carried out using surface hypothermia and inflow occlusion. Eleven of these patients were adults; the remainder were children aged 5 - 14 years.
more recollections from Tim Savage
| The first patient in this series was a 21yr old male, D.O., who had been admitted for cardiac catheterisation in April 1962. Ron Easthope was the HP, and the study was undertaken by Ponty Hallwright and Jeff Weston. The operation took place on 18/7/62, with cooling to 29.4 degrees C. and closure by direct suture. The surgeon was Jim Baird and the procedure took 7 hours. |
At Green Lane Hospital, surgery for pulmonary stenosis using deep hypothermia and circulatory arrest had been performed since 1953.
The first pulmonary valvotomy at Wellington Hospital was performed on a 2yr old old boy, S.R., on 8/5/63. He had been found at cardiac catheterisation six months earlier to have a RVP of 120mmHg. At operation, Jim Baird cooled the patient to 33.2 degrees C. and effected the valvotomy through an incision in the main pulmonary artery. This procedure took 4 hours.
A follow-up cardiac catheter performed by Ron Easthope in 1972 revealed a residual pulmonary valve gradient of 30mmHg. |
Preparations for cardiopulmonary bypass surgery at Wellington Hospital had been underway since July 1963.
| The patient selected for the first bypass operation was a 10yr old boy, P.C., with an atrial septal defect. He had undergone cardiac catheterisation in 1959 (technical difficulties), in 1962, and again in 1964 (because the ECG raised the possibility of a primum defect). A LV angio did not confirm the primum, but at the Combined Cardiac Clinic on 1/9/64, it was decided to list him for closure of the defect under cardiopulmonary bypass rather than hypothermia, because of the doubts raised by the conduction abnormality on the ECG. |
The team assembled for the first bypass operation included surgeons Jim Baird and Tim Savage, anaesthetist Murray Fergusson, and perfusionist Trevor Gebbie.
2/12/1964 : Closure of secundum atrial septal defect under bypass.
(L) femoral artery & vein cannulated.
Median sternotomy.
SVC & (with difficulty) IVC snared. (R) external iliac artery exposed, cannulated.
Defect 2.5cm x 1.5cm (finger exploration via RAA)
Partial bypass commenced; RA opened. Ventricles fibrillated with 1volt via needles in RV, but despite this, considerable coronary sinus return.
Defect closed by both continuous & interrupted sutures, though last suture not tied as residual defect acting as vent for (L) heart.
Unsuccessful attempts at defibrillation, using 100v & 150v AC - attributed to fact that temperature only 30 degrees. When 32 degrees, successful defibrillation using 150v AC.
Last suture tied. RA repaired
Initial partial bypass 1207hrs
Total bypass 1213 Rewarming 1238
Partial bypass 1255
Off bypass 1308 |
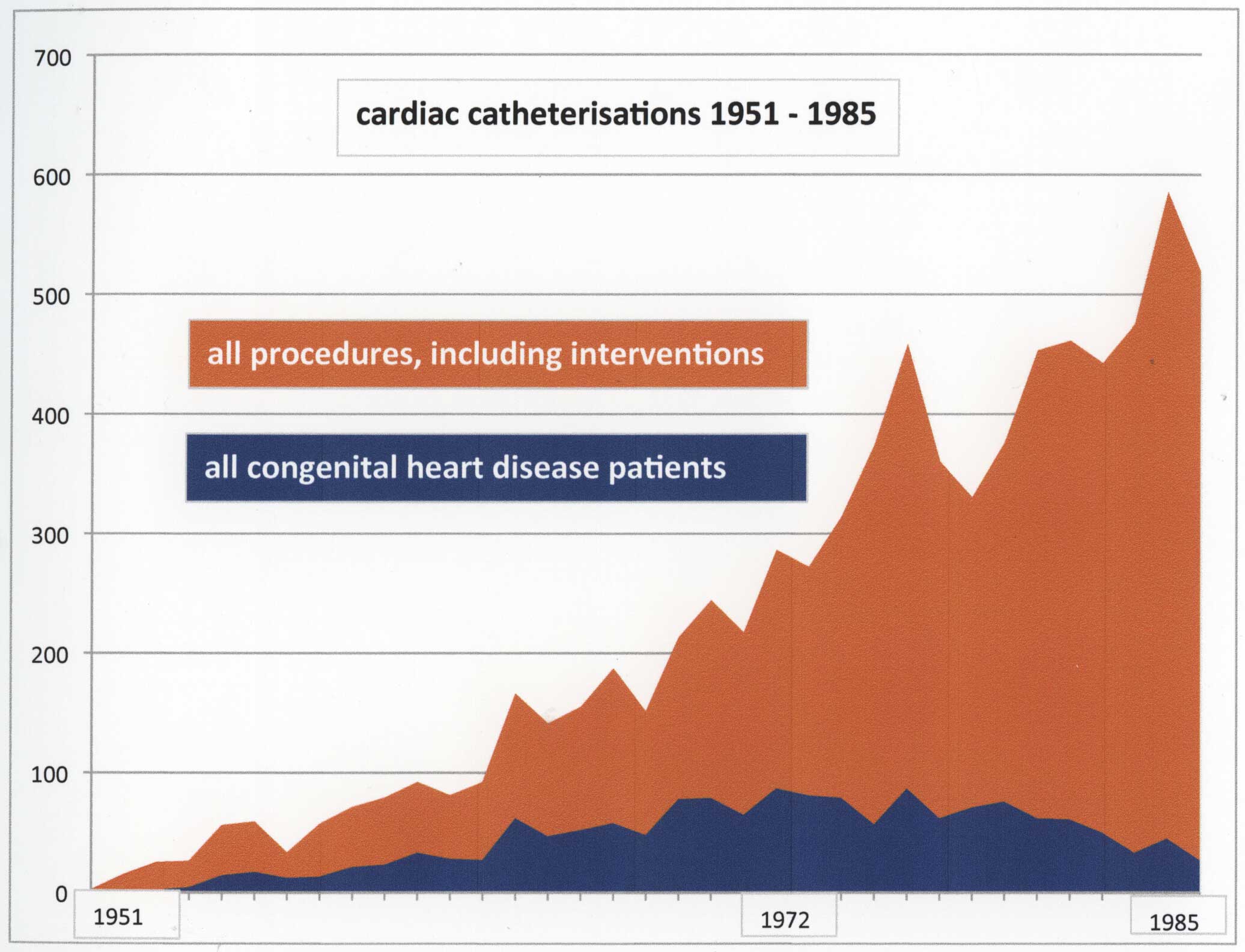
Many children and adults referred with congenital heart disease had accurate diagnoses made after clinical assessment aided by an ECG and chest xray. Cardiac catheterisation and angiography provided the level of detail required by the cardiac surgeons. Such patients constituted a significant proportion of the total cardiac catheterisation work load until the early 1970s. Peak numbers of cardiac catheterisations for congenital heart disease were achieved in 1972 and 1976 (87 annually), but by then adults undergoing coronary angiography began to overshadow them. From the early 1980s, the numbers of cardiac catheterisations for congenital heart disease started to fall away, and this is particularly evident from 1985. The availablilty of 2D echocardiography from 1984 was a big factor here.
A small but important part of the cardiac catheterisation service for congenital heart disease was in the neonatal age group. From 1962 - 1981, a total of 116 neonates (under 1 month of age) were studied by cardiac catheterisation.
Neonates with transposition of the great arteries often presented severely cyanosed and ill, typically when the ductus closed, and from 1969, balloon atrial septostomy became an option.
Prior to this there had been two attempts to surgically create an atrial connection (Blalock Hanlon procedure), one in 1966 (unsuccessful) and one successful operation was carried out in 1967.
Peter Leslie performed the first balloon atrial septostomy in 1969 and from then until 1981 a total of 33 such procedures were undertaken, either by Peter Leslie or Ron Easthope. Thereafter, duct-dependant neonates with cyanotic congenital heart disease were managed with prostaglandin therapy to maintain duct patency and then transferred to Green Lane Hospital for further evaluation and treatment.
From the late 1980s the majority of neonates with congenital heart disease and older children with relatively complex diagnoses were referred to the Green Lane team after intial clinical and echocardiographic assessment at Wellington Hospital.
After the initial experience with congenital heart disease surgery, Jim Baird ventured into undertaking more complex surgery. Diagnoses included VSD, Tetralogy of Fallot, complete AV Canal and septal defects with RV outflow obstruction at valve, infundibular and mid cavity sites.
Jim also had a brief and not too successful experience with the Mustard procedure for TGA. Three children aged 3 months, 4 years, and 7 months, underwent a Mustard procedure between November 1971 and April 1972. There was a gradual evolution of defining which patients were appropriate for surgery at Wellington Hospital and which patients should be referred to Green Lane Hospital.
Viewed in total, the cardiac surgeons in Wellington, including Jim Baird, Tim Savage, Bede Squire, Hedley Brown, Alan Hilless, Roger Franks and Ashok Sharma undertook 652 cardiac bypass procedures for congenital heart disease between 1964 and 1998, and roughly half of these were for atrial septal defects.
From the 1960s, congenital heart clinics were established to see new and follow up patients.
Peter Leslie and I each ran one clinic / month. For many years Jeff Weston provided valuable assistance in each of these clinics. The clinics were held within the Cardiology Department until the late 1990s when they were transferred to the OP rooms in the Paediatric Department.
In the late 1990s, the team at Green Lane Hospital initiated occasional visits by one of their number to coincide with these clinics. This provided an opportunity for selected patients who were potential surgical candidates to be seen in Wellington rather than travelling to Auckland for initial assessment.
Drs Nigel Wilson, Tom Gentles and Claire O'Donnell shared this visiting role.
After Peter Leslie and Ron Easthope retired, the responsibility for paediatric cardiology fell to Andrew Aitken. From early 2009, the venue for congenital heart disease clinics moved to the newly-opened CMU. The visits from the Auckland team have continued in this new location.