In the 1920s and 1930s, it was believed that people suffering acute coronary thrombosis could not survive. Admissions to hospital were rare, and such a diagnosis was generally made at autopsy.
Clinical diagnoses of acute myocardial infarction / coronary occlusion began to be made in the 1940s and especially in the 1950s. Realising that some of these patients could survive, measures were taken to improve outcomes, which in some cases had the opposite effect!
It became commonplace to insist that such patients be kept in bed for several weeks.
In 1952, there were 174 admissions with a primary diagnosis of acute myocardial infarction. There were 52 hospital deaths (30%) after a median 6 days in hospital. The 122 patients who were discharged alive had a median length of stay of 40 days.
These patients were admitted under the care of general physicians and there was no continuous ECG monitoring. Eventual ambulation was taken very slowly, and even after discharge from hospital, activities were significantly limited.
In hospital, morphine was used for pain relief together with nitroglycerine for interval angina. It was not uncommon for complications of prolonged inactivity in bed to occur, notably venous thrombosis and pulmonary embolism. It became fashionable in the 1950s to place all AMI patients on coumadin or dindevan, not just for venous thromboembolism prevention but also in the belief that there might be benefit at a coronary artery level.
The practice described above was still in place in the early 1960s - I well remember such patients when I was a house physician in 1961-62.
A new approach was introduced 1967, the coronary care unit. The concept of the CCU had been pioneered by Dr Desmond Julian who set up such a unit in Sydney in 1962. Key parts of the CCU concept included continuous ECG monitoring, the availability of immediate CPR if required, having an IV drip in situ, and prevention of thromboembolism.
Peter Leslie had the task of convincing Wellington Hospital's general physicians that patients presenting with acute myocardial infarction should be initially admitted to a CCU. Patients were to be admitted under the joint care of the general physician of the day and the cardiologist, and at an appropriate time, would be transferred to the relevant medical ward for convalescence.

The first four-bed unit in Ward 22 opened in 1967.
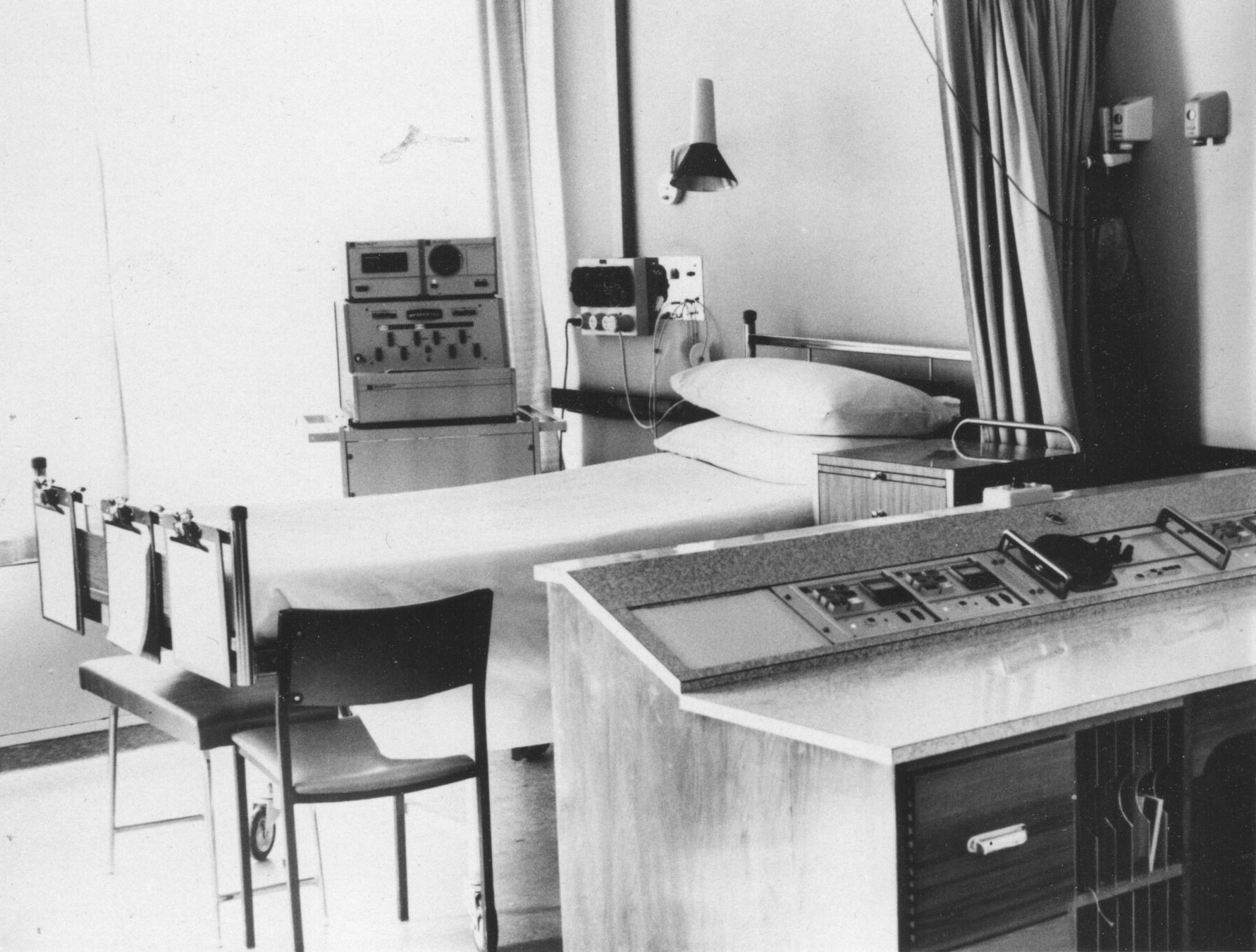
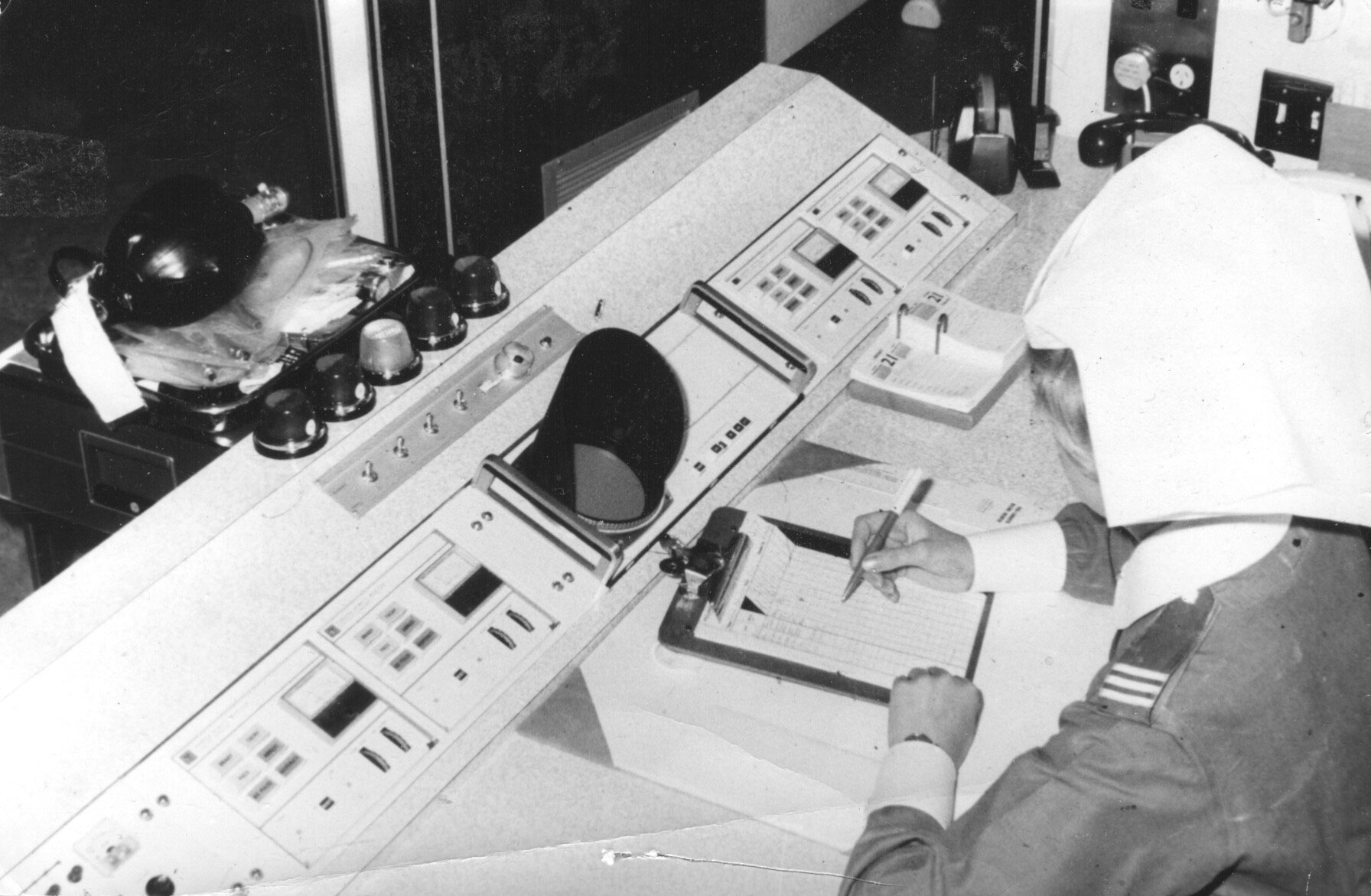
There were bedside monitors and a central monitoring desk.
ECG strips were recordable from the bedside monitor.
 There has never been a tidier desk!.
There has never been a tidier desk!.
In 1969 the unit moved to another four-bed cubicle in Ward 22 which had been modified to make each of the four beds located within an enclosed room. The vacated original 4-bed cubicle was converted to a renal dialysis unit.
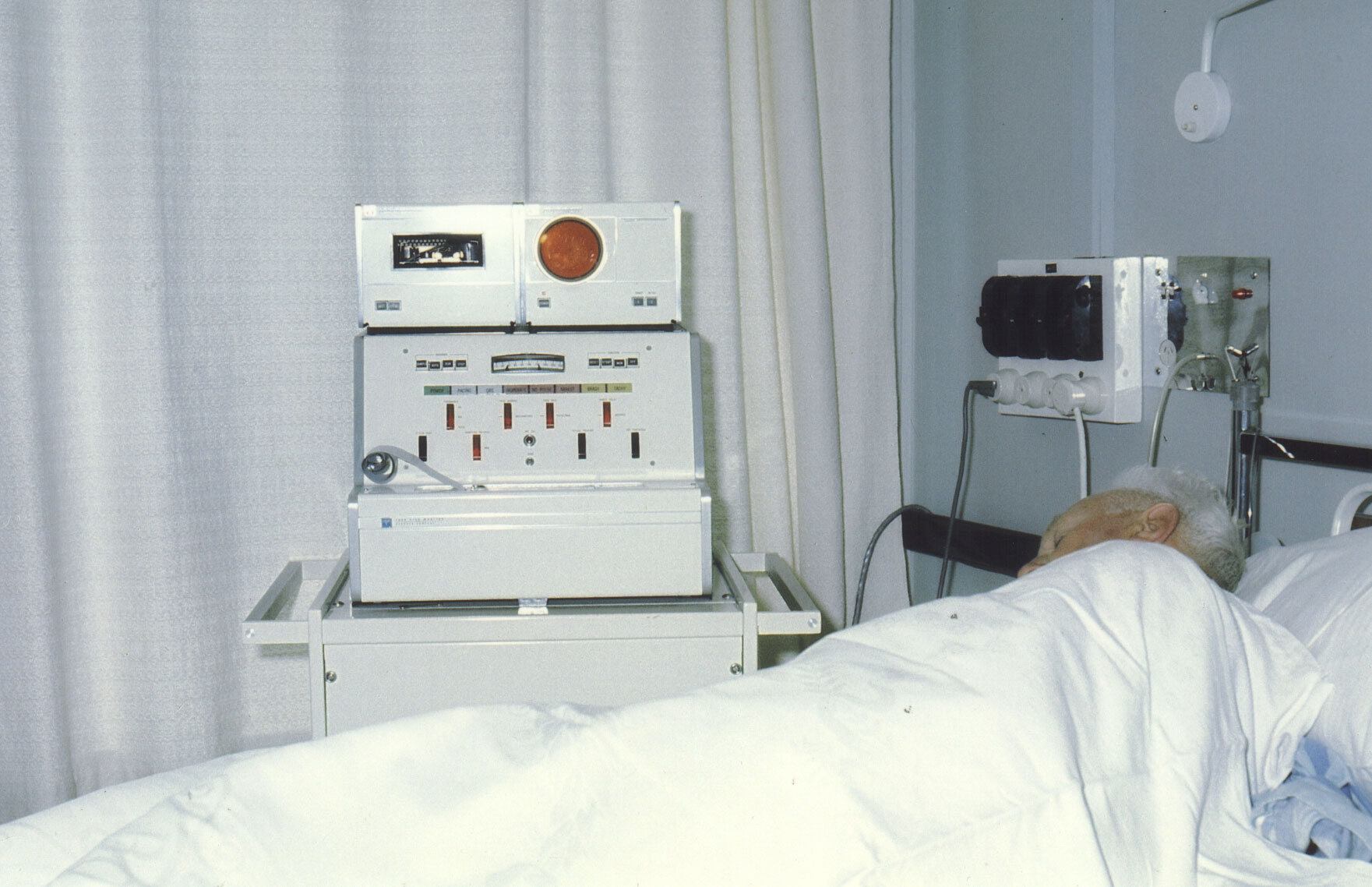
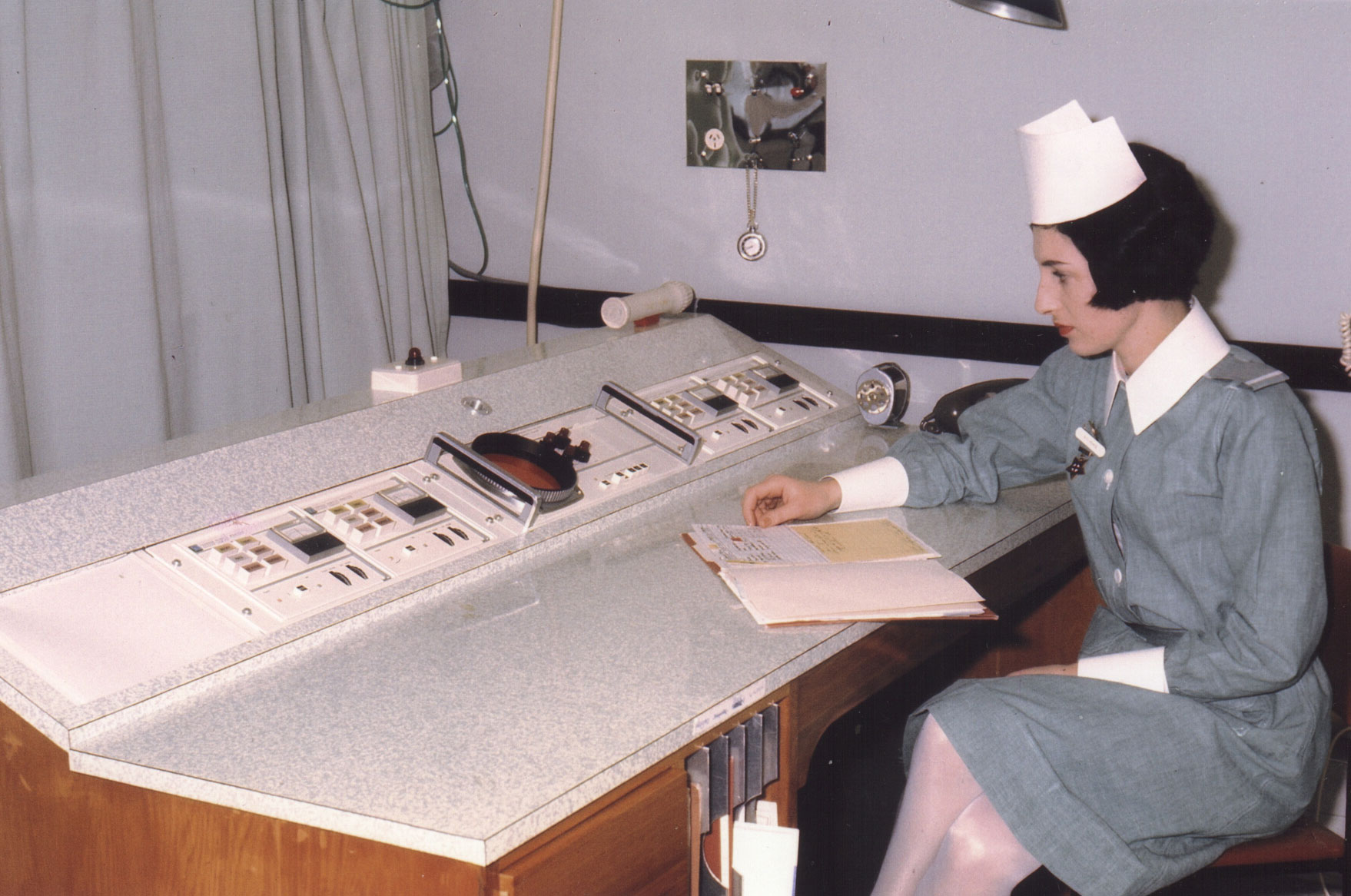
Below are photographs of the new unit just before it was occupied:
 the monitoring station the monitoring station | 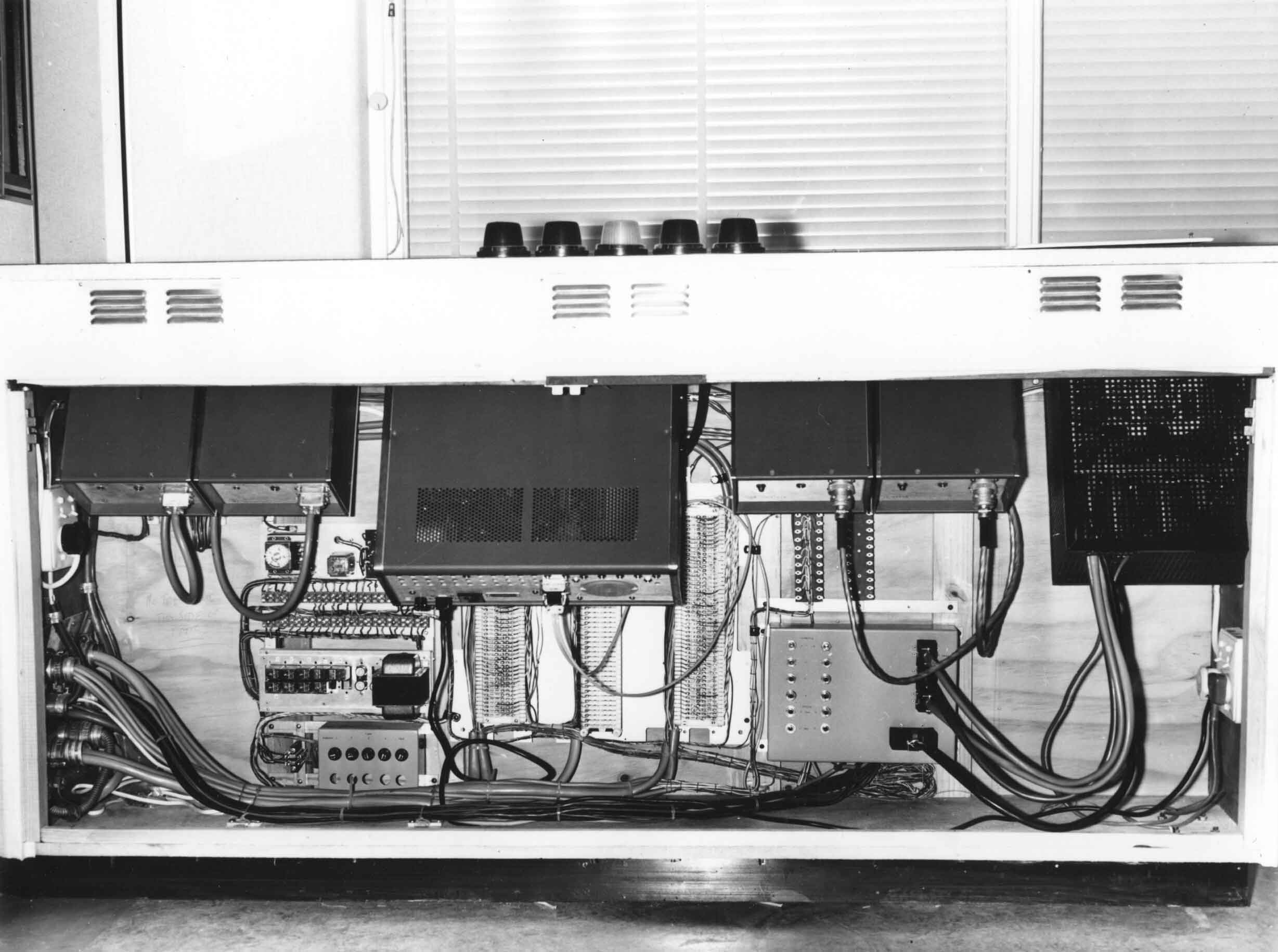 what's under the desk! what's under the desk! |
 cubicle 2 cubicle 2 | 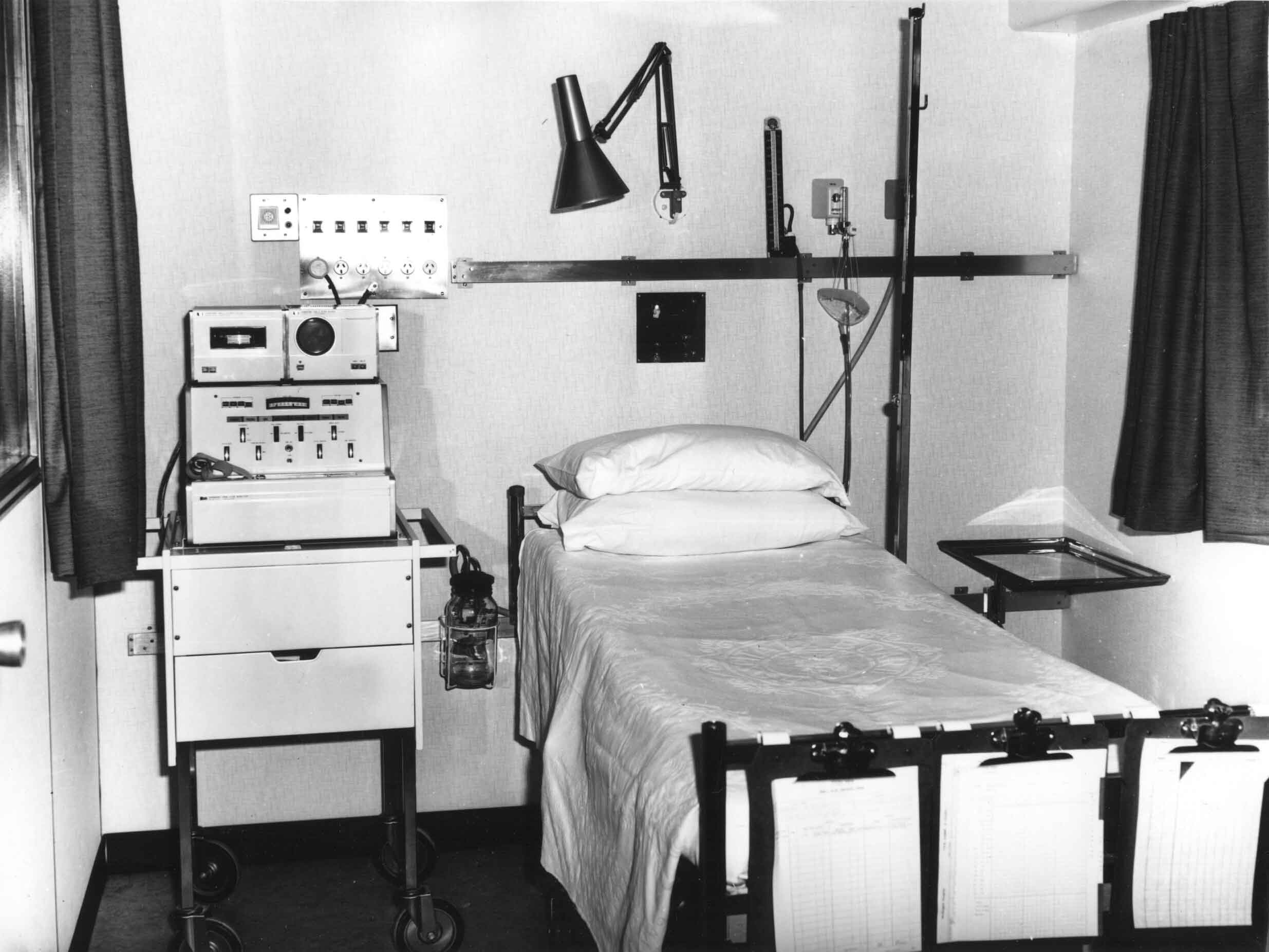 inside cubicle 2 inside cubicle 2 |
 X-Ray boxes and drug cupboard X-Ray boxes and drug cupboard |  inside the drug cupboard inside the drug cupboard |
 Sister Wendy Evans at work
Sister Wendy Evans at work
 Staff Nurse Diane Wilson studying an ECG strip
Staff Nurse Diane Wilson studying an ECG strip
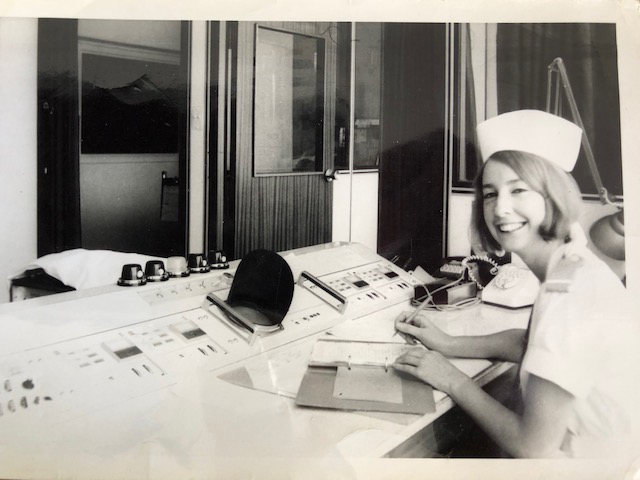
Staff Nurse Diana Hainsworth - very happy in her duties

In 1975 it became possible to receive ambulance-recorded ECGs in the unit. This was designed to give the ambulance staff confirmation that a patient in the community was in the process of having an acute myocardial infarction. It also gave unit staff warning that such a patient was on the way, and where appropriate, preparations for the administration of thrombolysis could begin.
By 1976, a new central monitoring console had been installed, this having improved monitors and ECG print-out capability.
 The CCU in the 1980s.
The CCU in the 1980s.
Newer and bulky central monitors - and a very 'busy' central monitoring station!
This rather cramped CCU remained in use, largely unchanged, for twentysix years.
However, during this time the number of monitored beds was increased by securing two beds in cubicle 12, and by the acquisition of telemetry units which allowed monitoring of additional patients elsewhere in the ward.
During the "Seddon era", some changes occurred in the management of patients with acute coronary syndromes.
Thrombolysis (streptokinase) in acute MI was used for the first time, and tPA became available soon after.
The availability of CABG surgery meant that there was another treatment option for selected patients who had presented acutely, not settled and were shown to have graftable vessels.
Symptom-limited treadmill testing of acute MI patients 6 weeks post-discharge was introduced to identify those who might need further assessment with coronary angiography. Later, low-level treadmill testing was introduced as a pre-discharge assessment, the main benefit of which was to give patients confidence in ambulation once home.
Length of stay in hospital came down so that after discharge from the CCU, patients often had only one or two more days in hospital. The general physicians had difficulty 'bonding' with these patients and there was a move toward remaining under the care of the cardiologist. However, limited bed availability made this impractable until after the unit moved from Seddon.
In 1993 a new Cardiac Care Unit opened on Level H, Ward Support Block.
This was the first such facility exclusively for cardiac patients, and the first specifically designed for that purpose.
Individual rooms for the more acutely ill were much roomier than in the Seddon CCU.

The new unit had seven 'hard-wired' monitored beds and there were six telemetry devices available to monitor selected patients in other cubicles.
Elective cardioversions were regularly carried out in the Cardiac Care Unit, typically in cubicle 6. For many years these procedures were done using IV valium for basal sedation, but eventually this was deemed to be an unsatisfactory practice and subsequent cardioversions required the presence of an anaesthetist.
The Cardiac Care Unit was still a long way from the Emergency Department which often meant that the duty cardiology registrar had to spend a lot of time in ED away from CCU. The cardiology HP became the go-to person on the ward.
Patients undergoing elective cardiac catheterisation were often preassessed in the CCU, the day before the planned procedure. These patients were admitted on the day of the investigation, being assigned one of the mobile beds located at the western end of the ward. They were transported to the cath lab on these beds, and post-procedure, returned to the ward to have the vascular access site monitored and await the cardiologist's report. Most of these patients were discharged the same day.
There have been improvements in thrombolytic therapy for acute MI. Both streptokinase and tPA are given as a 1-hour infusion. Newer agents such as reteplase and tenecteplase can be given by double or single bolus which is much easier for those administering the drug.
In 2000, the first percutaneous coronary interventions were undertaken for patients presenting with acute myocardial infarction associated with ST-elevation - STEMI. The 3rd patient so treated had been admitted from the Kapiti Coast. He had corporate connections and expressed his gratitude by arranging for his company to sponsor the provision of SIM cards for each of the latest LifePak devices in the Wellington Free Ambulance fleet. This allowed for the transmission of much better quality ECGs from ambulance to CCU.
From 2002, the ambulance service was trained and authorised to administer thrombolysis in the community to approved STEMI patients presenting on the Kapiti Coast. This has shortened the time to re-establishment of coronary patency for these patients.
Since the availability of newer high-sensitivity troponin assays, the spectrum of infarct presentation has changed. Significantly more patients with acute chest pain but without STEMI, are now troponin positive, and a number of these patients are receiving PCI on presentation. There are now fewer STEMI patients seen (around 50 - 60/yr).
On average there are 1 - 2 primary PCIs performed each week. The service is available 7am - 11pm, 7 days/wk, and it is hoped to make that 24/7 when an additional interventionist is appointed in early 2013.
A new CCU is part of the Wellington Regional Heart and Lung Unit, situated in ward 6 south in the new Wellington Regional Hospital. Transfer of the CCU from the ward support block occurred in early 2009.
The new unit has 8 'hard-wired' monitored beds - all single bed cubicles, together with two 2-bed cubicles in which telemetry can be used.
Elective cardiac catheter patients or those presenting electively for pacemaker implant are no longer preassessed in the CCU nor cared for there post-procedure. This now takes place wholly within the radiology facility where the cath labs are located.