Cardiac Surgery before Jim Baird's appointment
There has always been a strong and interdependent relationship between the two services, Cardiology and Cardiothoracic Surgery.
Before the arrival in Wellington of specifically trained surgeons, a small number of cardiac surgical procedures were undertaken.
1944 : R.B. - a young male admitted to ward 22 with a chronic febrile illness. Treated with sulphanilimide, (penicillin had yet to become available).
Noted to have a murmur. Charles Burns, the hospital's cardiologist was consulted.
A diagnosis of persistent ductus arteriosus with infective endocarditis was made. 
Charles Burns discussed the case with the Resident Surgeon, Herbert McNickle.
16 May, 1944. Ligation of infected PDA
Surgeon, Herbert McNickle assisted by Eric Luke
Patient fully recovered. |
This was one of the first operations in NZ for PDA; Five months later, Douglas Robb in Auckland would perform a similar operation for an infected duct, though that patient did not survive.

The next ductal ligation in Wellington occurred nearly 3 years after the first. On 21/2/1947, Richard Orgias, who had in 1946 succeeded Bert McNickle as Resident Surgeon, successfully operated on a young serviceman with an infected ductus. Dick Orgias was assisted in this operation by Eric Luke.
There were four more ductal ligations performed before Jim Baird's arrival, all performed by Dick Orgias.
The other type of cardiac surgery undertaken early related to the pericardium.
June 1944 K.G., a male was admitted to ward 8 with gross ascites.
Ponty Hallwright, who was assistant pathologist at this time, was known to have an interest in cardiovascular medicine and was asked to see the patient.
Based on the clinical findings and the chest xray, Ponty concluded that "he obviously had Pick's Disease".
In those days exposure times for chest xrays were significantly longer than they are today, so that most chest xrays showed a blurred cardiac silhouette due to cardiac movement.
However, in this case, the cardiac borders were sharply focussed.Once again, the Resident Surgeon, Herbert McNickle was consulted. 30 June, 1944
Pericardiectomy
Surgeon: Herbert McNickle assisted by David Whyte |
Two other pericardiectomies were undertaken in 1947.
One of these attracted some publicity - in the Dominion newspaper on 13/5/1947
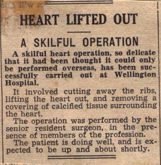
Appointment of first Cardiothoracic Surgeon
From the time of Jim Baird's appointment in 1952 as the hospital's first cardiothoracic surgeon, a close working relationship developed with the cardiology service. Given the personalities involved, the relationship was sometimes a little fraught in the early years but things settled down in time.
Tim Savage joined Jim as the second cardiothoracic surgeon in 1955.
A weekly meeting in the cardiology department between the cardiologists and cardiothoracic surgeons was held, at which cardiologists presented potential cardiac surgery candidates to the surgeons. If a referral was accepted the patient was wait-listed for surgery.
For the most part, these presentations were of patient histories and results of investigations, but in the early years, patients were often brought to the department on the day of the presentation. This allowed the surgeons to make a first-hand assessment of the surgical candidate. By 1963, seventyseven patients had been presented to the surgeons. The weekly meetings were referred to as the "Combined Cardiac Clinic".
Some historical detail of particular forms of cardiac surgery follows. Surgery for congenital heart disease is mentioned elsewhere.
VALVE SURGERY
Within three months of Jim Baird's appointment to the staff, he had performed the first closed mitral valvotomy. Jim had trained at the Brompton Hospital under Sir Russell Brock and O S Tubbs.
By the time Tim Savage arrived in 1955, Jim had undertaken twentythree such procedures.
The peak annual number of closed mitral valvotomies (21) was reached in 1969, but over the next ten years the frequency declined, and the last such operations were undertaken in 1979. Open mitral valvotomies were first carried out in Wellington in 1971 and became the norm after 1979.
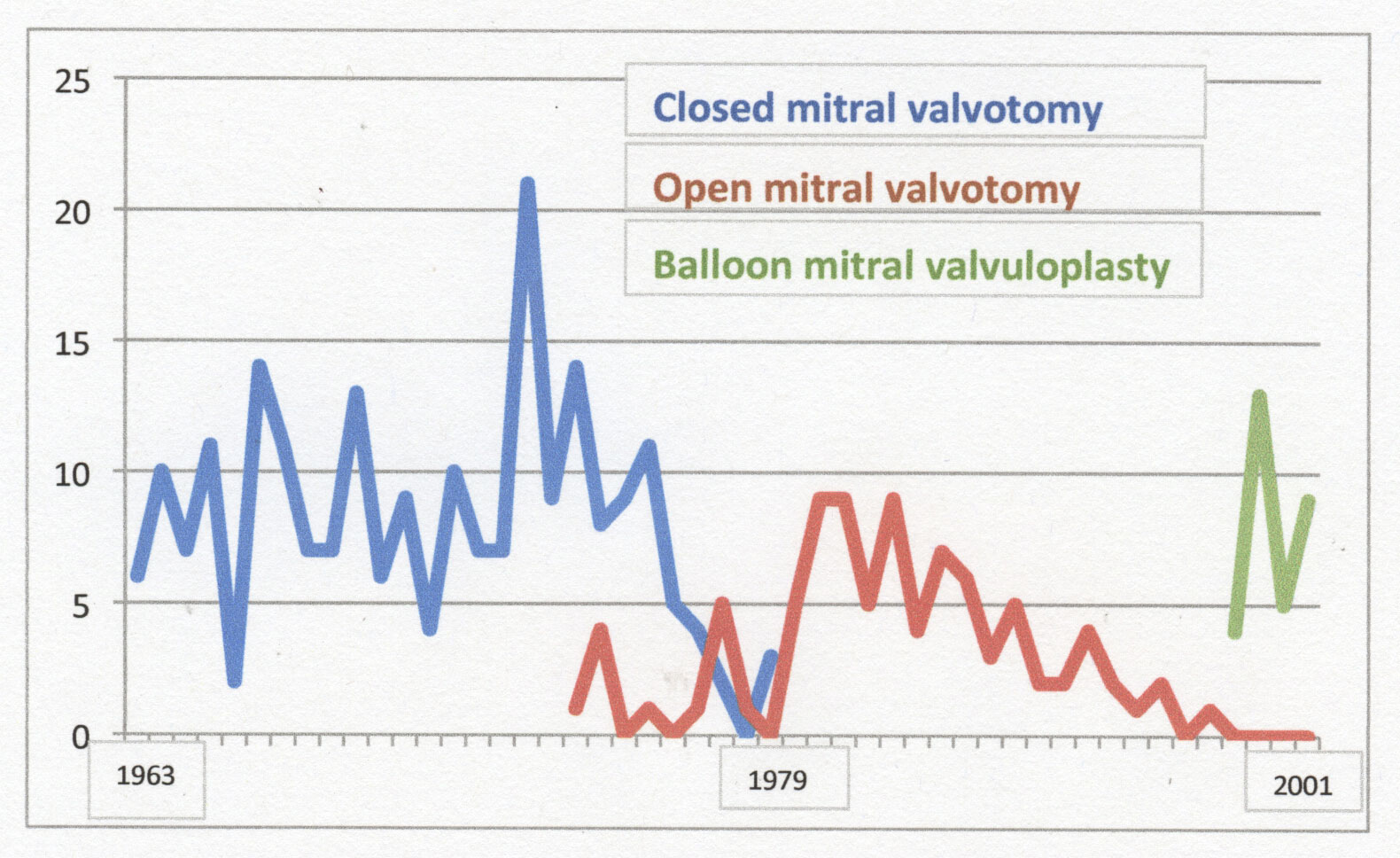 However, operative treatment of mitral stenosis gave way to percutaneous balloon valvuloplasty from 1998 (Phil Matsis).
However, operative treatment of mitral stenosis gave way to percutaneous balloon valvuloplasty from 1998 (Phil Matsis).
In 1960, Jim Baird spent six months in the UK and USA studying cardiac surgery. In the States in particular, his focus was on open heart surgery.
In 1963 Jim proposed that Wellington Hospital should become the second open heart surgery facility in NZ, and despite a late challenge from Dunedin (who wanted the facility to be there), the Minister of Health announced on 4 July, 1963 that Wellington Hospital's bid was approved. Detailed planning for the unit followed, including regular animal surgery to familiarise and test out the new techniques. The first cardiopulmonary bypass procedure (closure of an ASD) was undertaken in December, 1964.
By the time of the first valve replacement operation, 48 cardiopulmonary bypass procedures had been undertaken.
D.V., a 48 yr old man, presented with severe aortic regurgitation and congestive cardiac failure. Cardiac catheterisation 6/10/1966 (Peter Leslie) Severe AR confirmed plus pulmonary hypertension. He was selected to be the first candidate for aortic valve replacement. 13/12 1966 Homograft aortic valve replacement. Surgeon Jim Baird, assisted by Tim Savage. Operation started 8.30am. Operation completed 7.00pm Patient died 24hrs later. |
The choice of a homograft valve was no doubt influenced by the successful use of such valves at Green Lane Hospital. Homograft valves were used in only three subsequent aortic valve replacements, in 1967, 1968 and 1969.
The second aortic valve replacement was carried out in March 1967.
K.T., a 44 yr old man had presented in 1966 with effort syncope and was found to have severe aortic stenosis.
Cardiac catheterisation 21/9/66 (Peter Leslie)
Aortic valve gradient 60mmHgPatient accepted for aortic valve replacement. Starr-Edwards aortic valve replacement 14/3/67
Surgeon Jim Baird assisted by Tim Savage.
Operation started 8.30am Operation completed 7.45pm
Major haemorrhage from suture lines requiring massive transfusion.
Poor output postop, requiring peritoneal dialysis from day 3;
Died one week post-op. |
This was clearly a disappointing start to the valve replacement programme, but the surgeons were committed to continuing and a further 28 patients were operated on in 1967.
Most of the early valve replacements were aortic but the first mitral valve replacement took place in June 1967.
P.C. was a 38 yr old man who underwent a closed mitral valvotomy (Tim Savage) in 1959.
Adverse features were calcium in the mitral valve and thrombus in the LA.
He had an episode of pulmonary oedema in 1965.
6/6/1967: Starr-Edwards MVR
Surgeon Tim Savage assisted by Jim Baird.
Thrombus in LA.
Operation commenced 8.30am. Operation completed 4.30pm. |
He remained reasonably well until 1988 when he developed prosthetic endocarditis. He underwent an urgent MVR (Alan Hilless) on 23/8/88, had a protracted post-op course, and died on 28/10/88.
The second MVR was carried out one month after the first.
G.C., a 66 yr old woman had severe mitral regurgitation and pulmonary hypertension.
4/7/1967: Starr-Edwards MVR
Surgeon Jim Baird assisted by Tim Savage.
Operation started 8.30am Operation completed 3.30pm
Protracted post-op course but discharged on 30/9/67. |
Here is a cardiac surgical procedure underway in the Seddon Theatre, with surgeons Jim Baird, Tim Savage and Bede Squire all scrubbed.

In time, valve replacement surgery results improved, in part as a result of better patient selection.
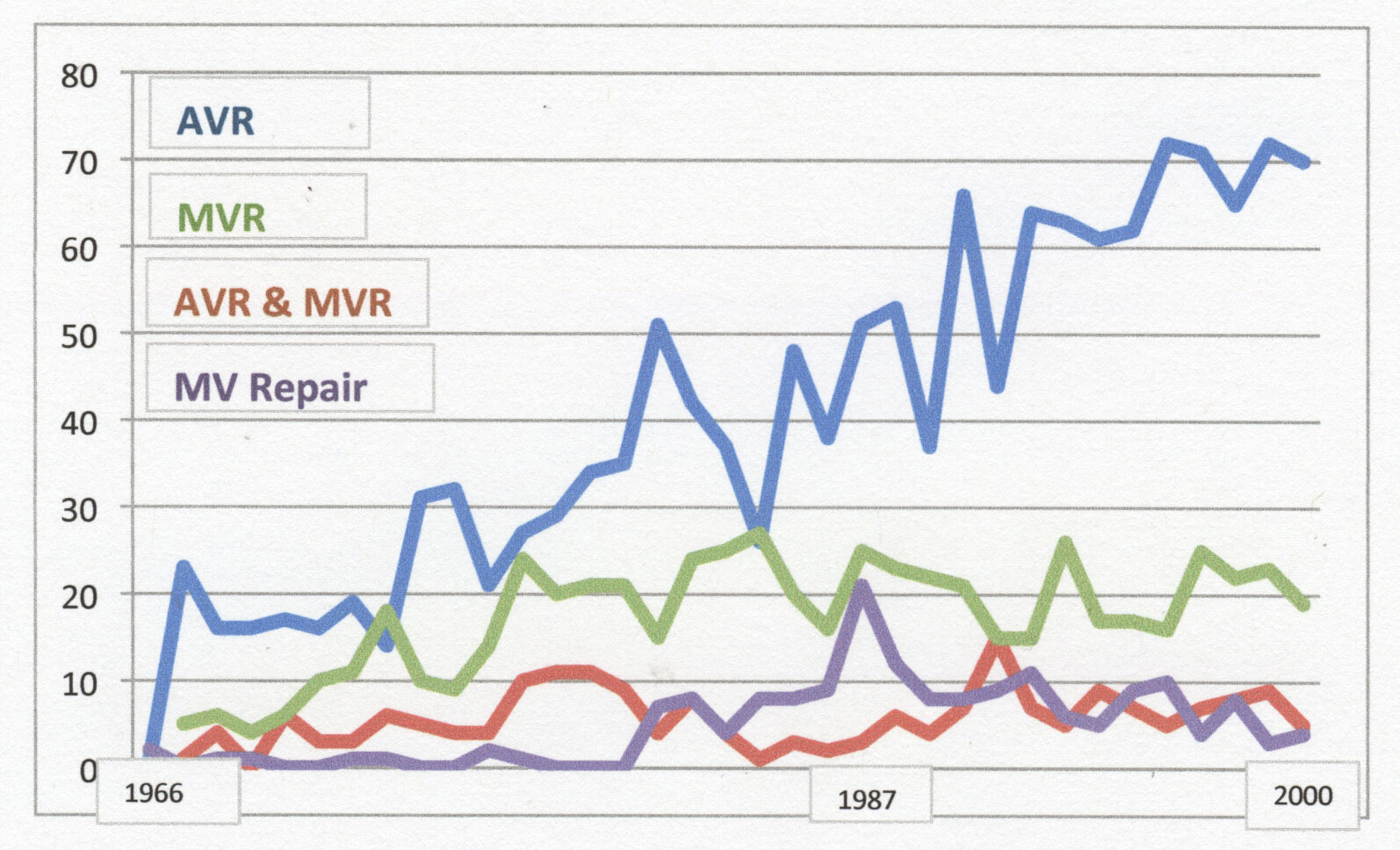
Numbers of aortic valve replacements have steadily increased, whereas mitral valve replacement numbers reached a plateau. Mitral valve repair has played a part here.
CORONARY DISEASE SURGERY
It will come as a surprise to some that we need to go back to 1938 to learn about the first surgery undertaken for coronary disease at Wellington Hospital.
W.C. was a 53 yr old man who had been in ward 7 for months, seemingly bedridden with intractable angina.
In October, 1938, Fred Bowerbank was consulted, and he in turn, had discussions with Dr John Cairney.
14/10/1938: Cardio-omentopexy - pedicled omental graft applied to the anterior wall of the LV.
Surgeon: John Cairney. Anaesthetist: Eric Anson
Within a few weeks of surgery, patient mobile and angina-free.
Discharged after 149 days in hospital. |
This operation had been pioneered by a brilliant young British surgeon, Lawrence O'Shaughnessy. In a letter written to me in October 2002, Verney Cable mentioned:
"I saw the first English heart operation - a pushing, eager young surgeon who knew that angina was a consequence of defective myocardial blood supply, so he opened the abdomen of an anginal patient, took the delicate peritoneal apron which hangs from the outer curvature of the stomach and which has small arteries and veins in it, incised the diaphragm and sewed this on to the heart."
At the time, Verney was HP at the City of London Hospital for Diseases of the Heart and Lungs, Victoria Park.
Fred Bowerbank was in London in late 1937 on study leave. Whilst there, he made two visits to the Lambeth Hospital to watch O'Shaughnessy carry out cardio-omentopexy operations, and he also attended an evening meeting at which O'Shaughnessy described the operation. Bowerbank returned to Wellington in 1938, and so it comes as no surprise that he suggested such an operation for the patient just described.
Ten months after that first operation, another patient with angina presented.
V.B., a 49 yr old man was admitted to ward 7 with severe angina.
On 18/8/1939, a cardio-omentopexy operation was performed.
Surgeon: S D (Tommy) Rhind, assisted by John Cairney.
Patient died after a hospital stay of 69 days. |
No further such procedures were carried out at Wellington Hospital.
To find the next instances of surgery for coronary disease we need to jump forward nearly thirty years.
J.O'B., a 49 yr old man was admitted with intractable angina
19/12/67: Coronary angiogram (Peter Leslie): diffuse RCA disease and occluded LAD
1/7/68: Vineberg procedure - bilateral internal mammary artery implants on to LV.
Surgeon: Jim Baird.
Operation commenced 8.00am Operation completed 2.00pm.
The patient was free of angina for the next six months. |
On 14/10/1968, Ponty Hallwright wrote to me whilst I was in London:
"Peter has got the Vineberg bug, but not badly, and I have great difficulty in accepting this technique in the absence of satisfactory controls in other parts of the world. I had demonstrated to me some good results in Cleveland and elsewhere but much more is needed before we can accept this fairly considerable procedure."
The first Wellington Vineberg patient redeveloped angina in 1969.
8/5/75: Coronary angio (Peter Leslie): Severe three vessel disease
8/10/75: CABG x4
Surgeon: Bede Squire.
Patient angina-free through to April 1976, and subsequently LTFU. |
One further Vineberg operation was performed at Wellington Hospital.
J.P., a 24 yr old male with familial hypercholesterolaemia was referred to Peter Leslie.
He had first presented in 1966 at the age of 19 with a myocardial infarction.
Unstable angina.
12/6/69: Cardiac catheterisation (Peter Leslie)
Diffuse 3-vessel disease.
10/3/70: Vineberg procedure. Surgeon: Jim Baird.
Less angina two months later.
1970 - 1971: x4 admissions with unstable angina.
25/2/77: Referred Green Lane Hospital (from Waikato). After repeat coronary angiography, accepted for CABG surgery, but later LTFU. |
The first coronary artery bypass graft operation at Wellington Hospital was performed in 1972.
F.van H., a 50 yr old man had recurrent admissions with unstable angina in 1971 and 1972.
1/2/72: Coronary angiogram (Peter Leslie)
Occluded LAD and RCS; severe disease in circumflex.
24/3/72: CABG, vein grafts to LAD and to RCA.
Surgeon: Jim Baird.
Operation started 8.50am Operation completed 7.20pm.
Total bypass time: 145mins. |
Angina-free for a few months.
27/6/72: admitted with unstable angina.
Coronary angiogram: subtotal obstruction graft to RCA; narrowed graft to LAD.
Managed medically.
Stable angina through 1976, but sudden death in December of that year. |
Jim Baird undertook the next four CABG procedures, all in 1972 and one more in 1973 before deciding that he did not want to be involved with that form of surgery.

Bede Squire had joined the team in 1968 and he began CABG surgery in late 1972.
Total numbers of CABG procedures remained low however, with seven in 1972 and just four in 1973.

Hedley Brown was appointed the fourth cardiovascular surgeon in 1973, and he upped the tempo.
The frequency of CABG surgery significantly increased from 1974, and Hedley performed a majority of these procedures.
Hedley remained on staff until 1978.
Thereafter, from May 1978 until July 1979, all CABG surgery was done by Bede Squire. During this time Bede carried out 100 CABG operations.
The CABG workload increased considerably from the mid 1970s as large numbers of patients were referred from Christchurch Hospital (which did not have cardiac surgery locally). Such referrals continued through to the early 1980s. Sixtyeight Christchurch patients were operated on in 1980.

Alan Hilless joined the staff in July 1979 and the workload became better distributed.
Early in the CABG programme, the vast majority of patients received saphenous vein grafts, though it became relatively common for surgeons to use the (L) internal mammary artery for LAD grafts. Subsequently, a number of international studies reported better long-term graft patency rates when arterial grafts were used, and from the late 1980s there was a move toward using radial artery conduits more often, not just when there were no suitable veins.

Roger Franks joined the surgical staff in 1984 and particpated in all forms of surgery.

Ashok Sharma arrived in 1988 and he was an enthusiastic user of arterial grafts.
Ashok also pioneered in Wellington the technique of minimally invasive ("off pump") CABG surgery in selected patients. Between 1996 and 2000, Ashok performed 32 such procedures.