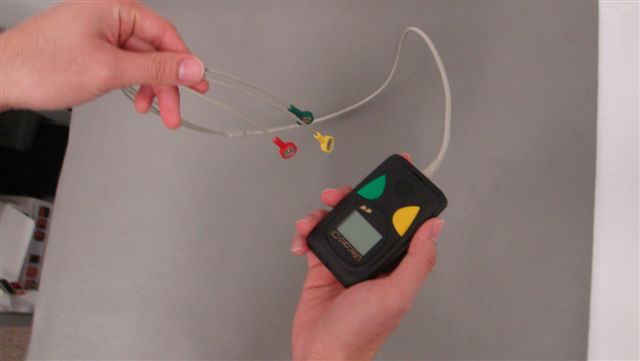
Shown here is one of the ECG machines in current use in the Clinical Measurenet Unit.
The original ECGs recorded using a string galvanometer were captured photographically. The photographs were processed in a dark room and the prints cut into narrow strips which were pasted on to a card, or in later years, mounted using staples.
This ECG was recorded in 1955, and was probably one of the last photographic tracings made.
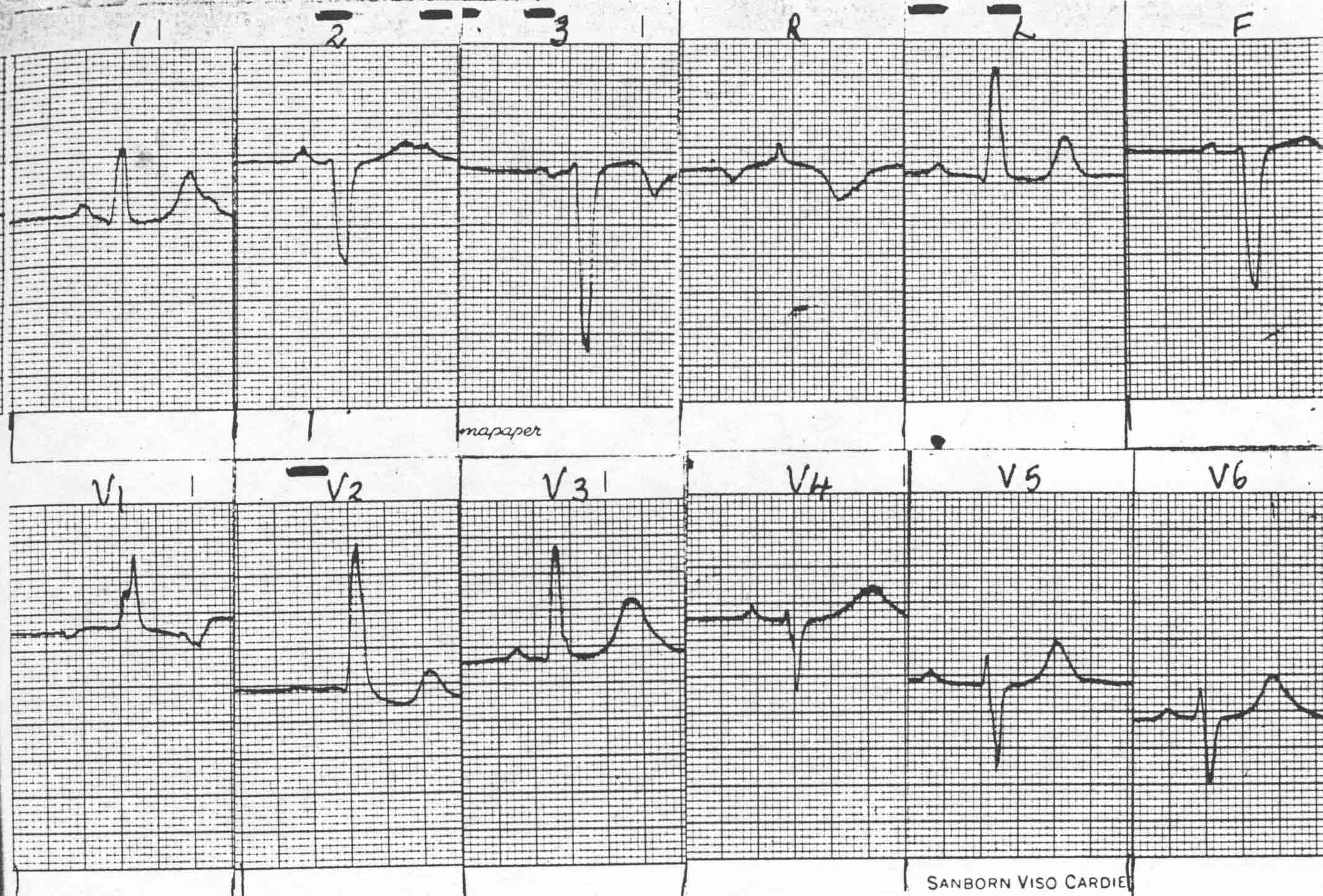 With the acquisition of the Viso Cardiette electrocardiograph, came a major advance in ECG processing. No longer was a dark room required. The paper output was marked to label each ECG lead sample, and the unmounted ECG was attached to the request form and placed in a basket for reporting.
With the acquisition of the Viso Cardiette electrocardiograph, came a major advance in ECG processing. No longer was a dark room required. The paper output was marked to label each ECG lead sample, and the unmounted ECG was attached to the request form and placed in a basket for reporting.
Before mounting, selected examples of each ECG lead, together with a sample of continuous record (for rhythm), were laid on heat-sensitive glued paper. Then, a warm iron was applied to activate the glue and thereby fix the mounted ECG samples.

This was a very time-consuming process, and in the 1970s a clerk was employed to assist in mounting, thus freeing the technicians for other duties. One such clerk was Val Burke, pictured left.

In 1977, Betty Cosgrove joined the staff in this role which also included answering phone calls to the technicians' work room. During Betty's tenure, double-sided sticky tape became available and the cumbersome mounting irons were consigned to history. Betty retired from the Cardiology Department in 1990.
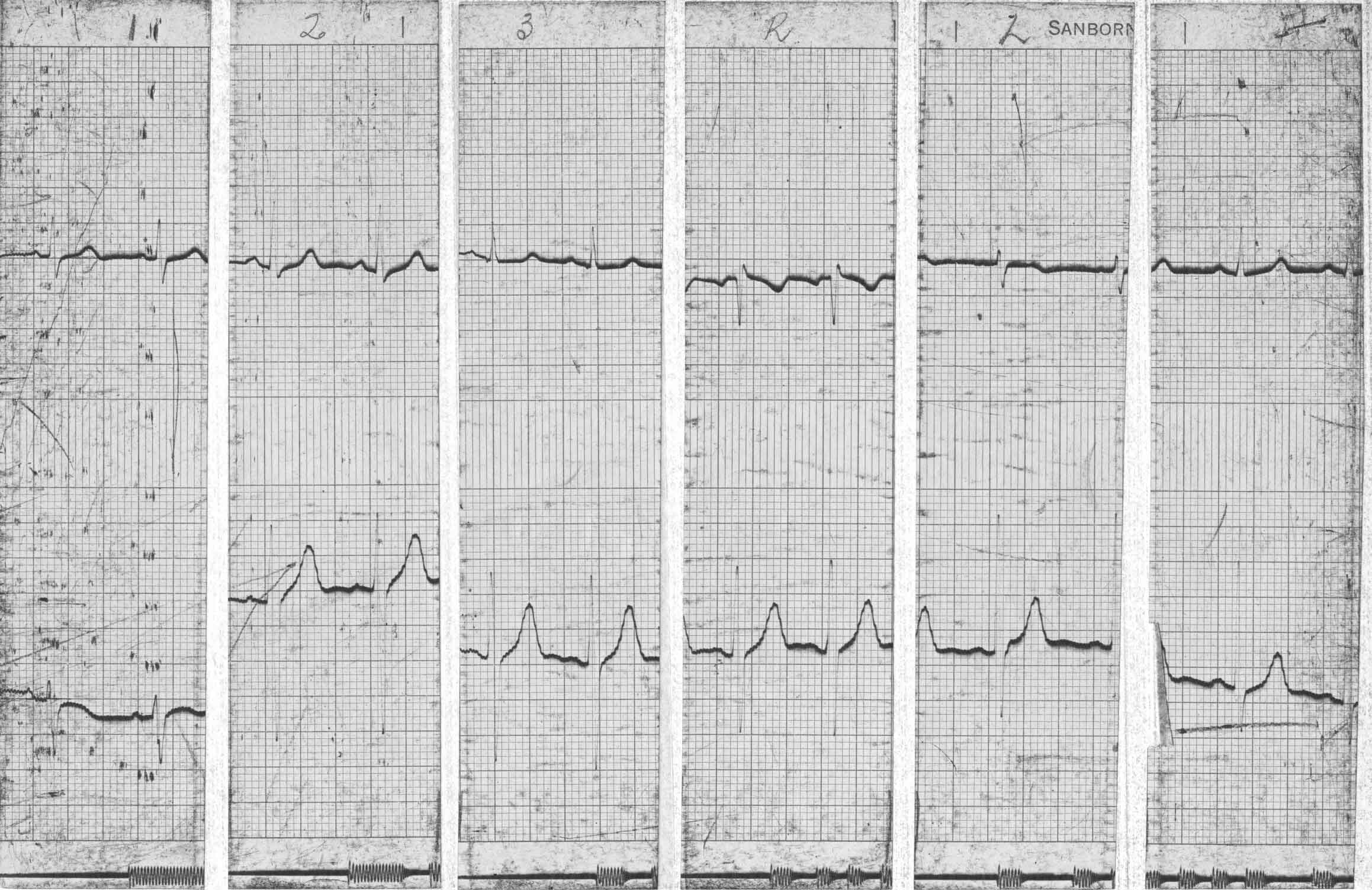
With the acquisition of a 2-channel electrocardiograph, some processing time was saved by having paired leads printed simultaneously.
Once pagewriter ECG machines came on the scene, mounting of ECGs was no longer required.
ECG Reporting
Fred Bowerbank would have reported all the ECGs done during his tenure.
In 1948, Charles Burns observed that the number of ECGs being done had significantly increased and that he spent the equivalent of one half-day each week reporting them. He was not being reimbursed for this work.
Eventually there was recognition of the time spent reporting ECGs and by the early 1960s, four physicians (Drs Hallwright, Hall, Todd and Luke) were each paid for one ECG reporting session/week.
ECG reporting was always something of a chore, not helped by the lack of clinical detail supplied by the requestor in some cases. Some of the reporting physicians collected the large pile of ECGs at the end of the day, took them home for reporting, and returned them the following morning. Others, such as Frank Hall preferred to report the ECGs in the Department during the evening. On more than one occasion I remember well attending the department during the evening when on-call and finding Frank Hall fast asleep over a pile of ECGs at his desk!
With the arrival of full-time cardiologists, Ponty Hallwright was the first to be let off the ECG reporting hook.
During the 1960s and 70s, all ECGs recorded in the hospital, including those done on ECG machines based out of the Cardiology Department, were required to be reported by cardiology staff. There was subsequently a move toward general and other specialist physicians and their registrars reporting ECGs on their own patients. Eventually, cardiology staff reported only ECGs from surgical wards, the Emergency Department and those requested by GPs.
Ambulatory ECG Monitoring
The first Holter monitoring equipment was acquired in 1979. It was an Oxford Medilog, tape-based system which provided limited display of rhythm abnormalities on a very small screen, and an ECG strip needed to be printed out for each suspected abnormality.

The second Holter recording system was acquired on 31/10/1984, financed in part by a generous grant from the Watson Trust.
The total cost of the Oxford Medilog equipment was $33,000. In the photograph below are Charge Technician Gwen Turner and Technician Vikky D'Ath with a patient.
 This new Holter system was a big improvement over the first in that the analysis screen was large and full rhythm strips could be viewed.
This new Holter system was a big improvement over the first in that the analysis screen was large and full rhythm strips could be viewed.

The Oxford Holter monitoring system proved to be a useful tool though problems with malfunctioning of the tape system were not infrequent.
In 1992, a Del Mar digital system replaced the Oxford tape-based equipment, and no longer were there any problems with tapes sticking. In addition, the analysis software was more sophisticated.
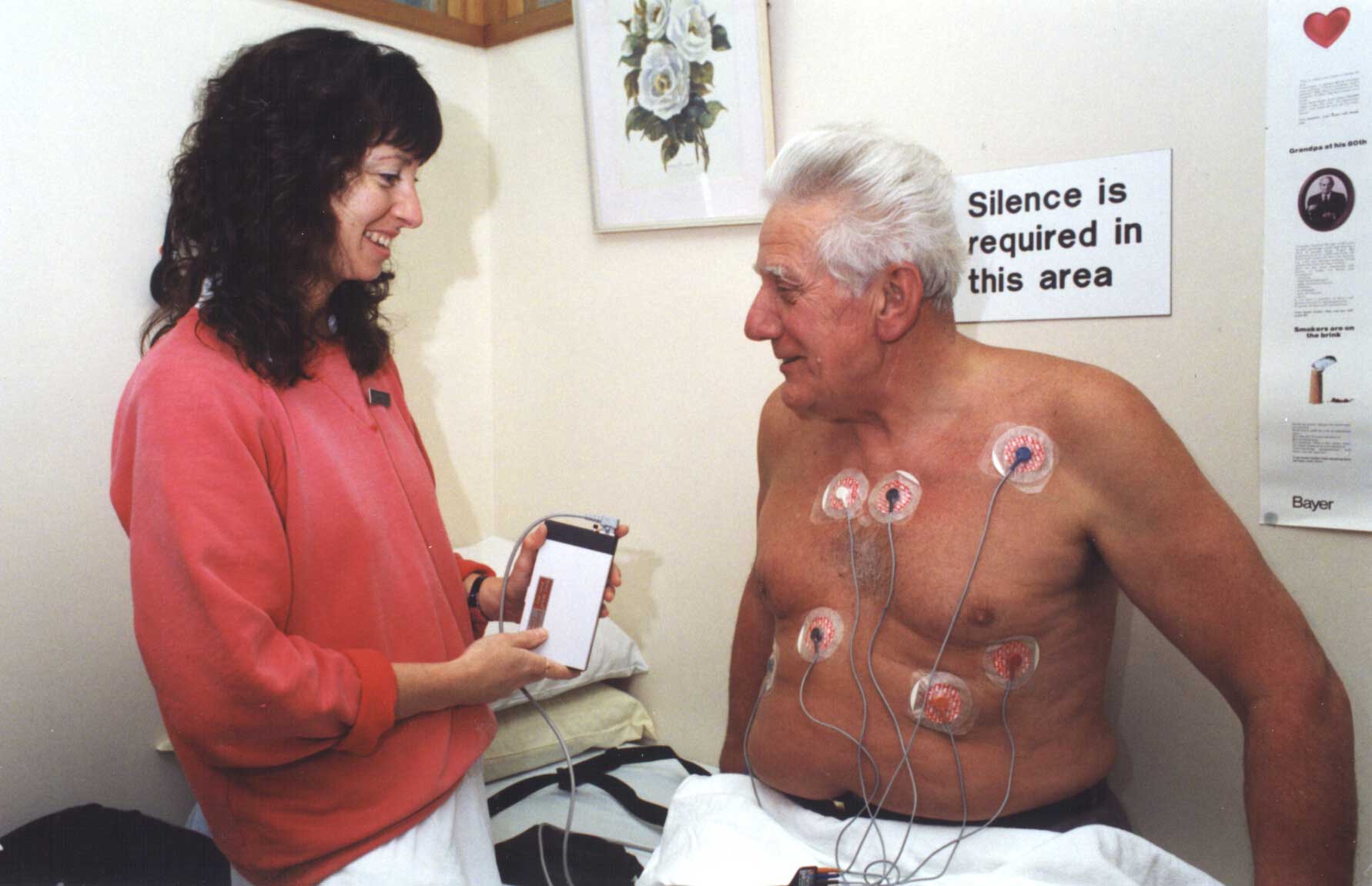
Here Technician Susan Brady explains the procedure to a patient.
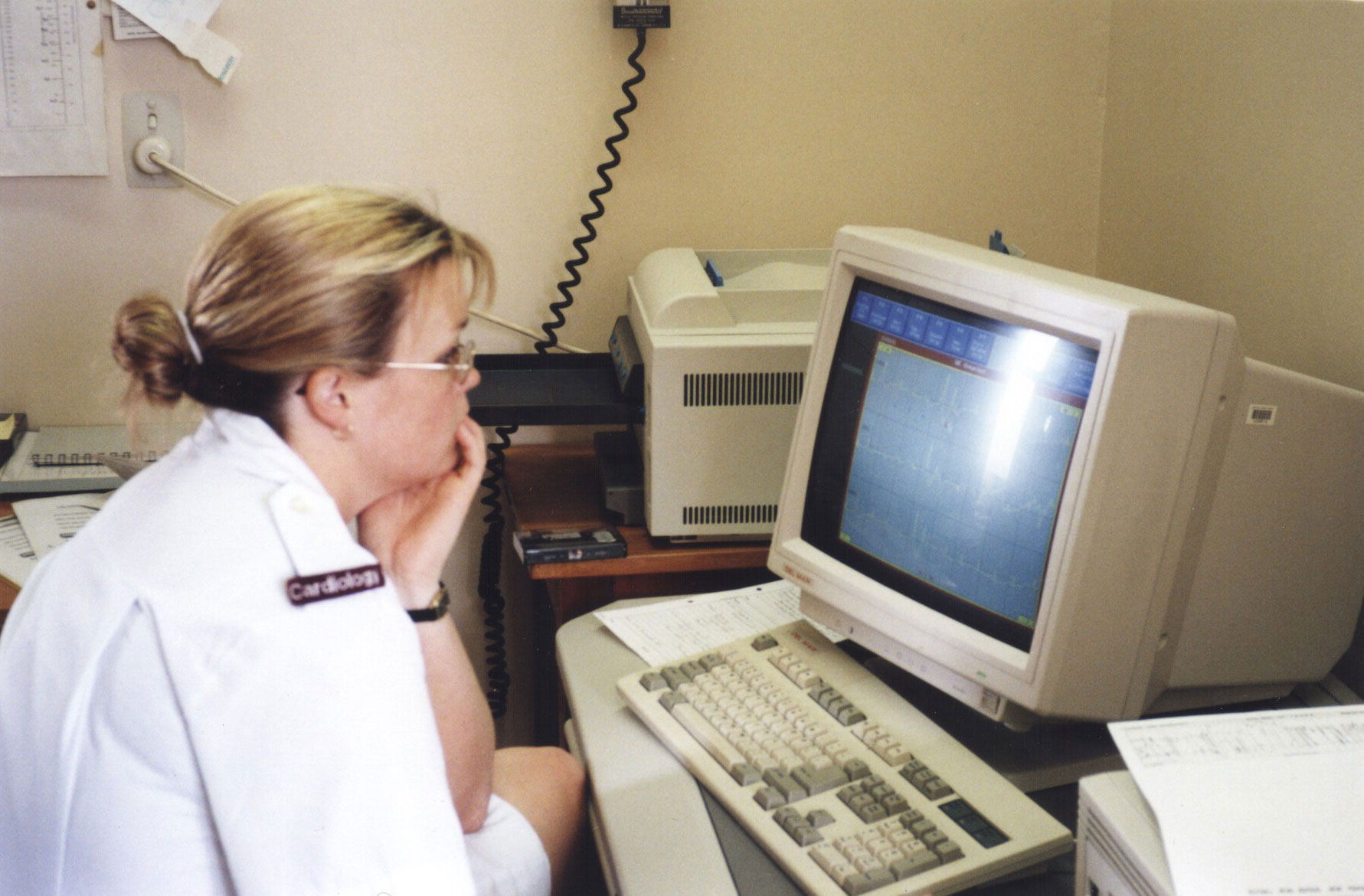
Technician Talia Canvin analysing a 24-hour recording acquired with the new system
A newer Del Mar Holter system was acquired in 2008, with smaller patient recorders and an improved digital recording system.
In 2001 the first implantable ECG recorder was used - the Medtronic Reveal.
