The first cardiac catheterisation was undertaken by Verney Cable on 14/12/1951. This was a (R) heart study on a 27yr old man with CCF. He died two months later and at autopsy was found to have a dilated cardiomyopathy. (It is likely that this investigation was done to exclude pericardial disease.)
Verney undertook at total of 14 procedures, all (R) heart studies, the last on 25/8/1953.
This patient group comprised:
- 7 patients with mitral stenosis
- 5 patients with CCF
- 1 patient with Tetralogy of Fallot
- 1 patient with a persistent ductus arteriosus
Marshall Luke, who was a medical registrar at that time, recalls Verney Cable's excitement on 11/1/1952 (cather #3) when the catheter passed direct from RV to ascending aorta in a 21yr old man with Tetralogy of Fallot.
Cardiac Catheter Lab location
The earliest investigations were undertaken in Room C, situated within the X-Ray Department, access to which was down a ramp off the hospital corridor.
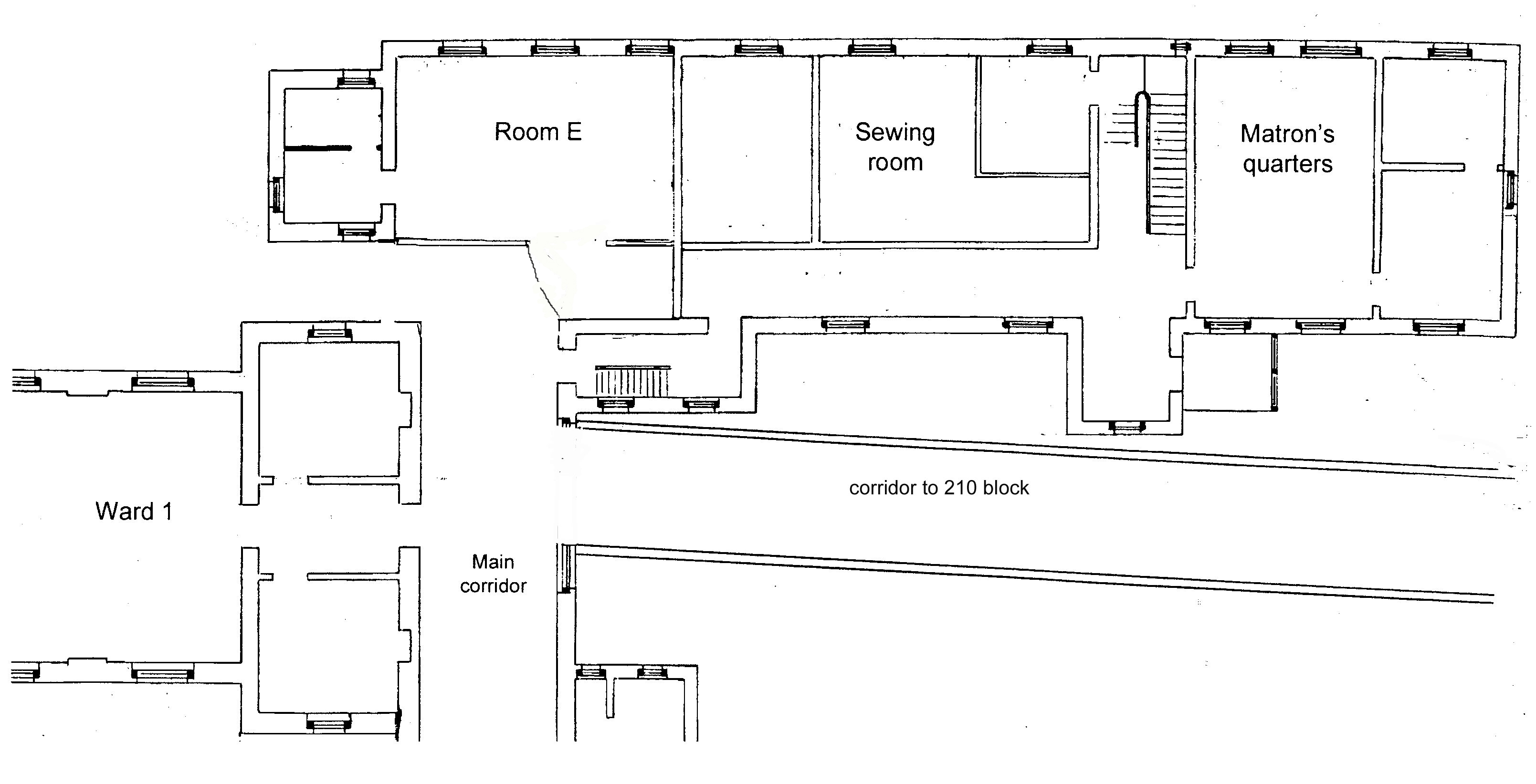 A move to Room E occurred in 1958. This room was in the southern end of the ground floor of the 'Matron's Block', just off the western end of the old main corridor. [Prior to the opening of the Main X-Ray Department in 1913, the 'Room E' site had been the hospital's first and only X-Ray Department, created in what had been the original children's ward prior to the opening of the King Edward VII Memorial Hospital for Children in 1912.]
A move to Room E occurred in 1958. This room was in the southern end of the ground floor of the 'Matron's Block', just off the western end of the old main corridor. [Prior to the opening of the Main X-Ray Department in 1913, the 'Room E' site had been the hospital's first and only X-Ray Department, created in what had been the original children's ward prior to the opening of the King Edward VII Memorial Hospital for Children in 1912.]
 In the photograph of Room E above, 'Big Bertha' in its original configuration is centre-back.
In the photograph of Room E above, 'Big Bertha' in its original configuration is centre-back.
 The opening of the new Seddon Block in 1966 saw a move to a purpose-built cardiac catheter lab, on the same level as ward 22, the cardiology ward.
The opening of the new Seddon Block in 1966 saw a move to a purpose-built cardiac catheter lab, on the same level as ward 22, the cardiology ward.
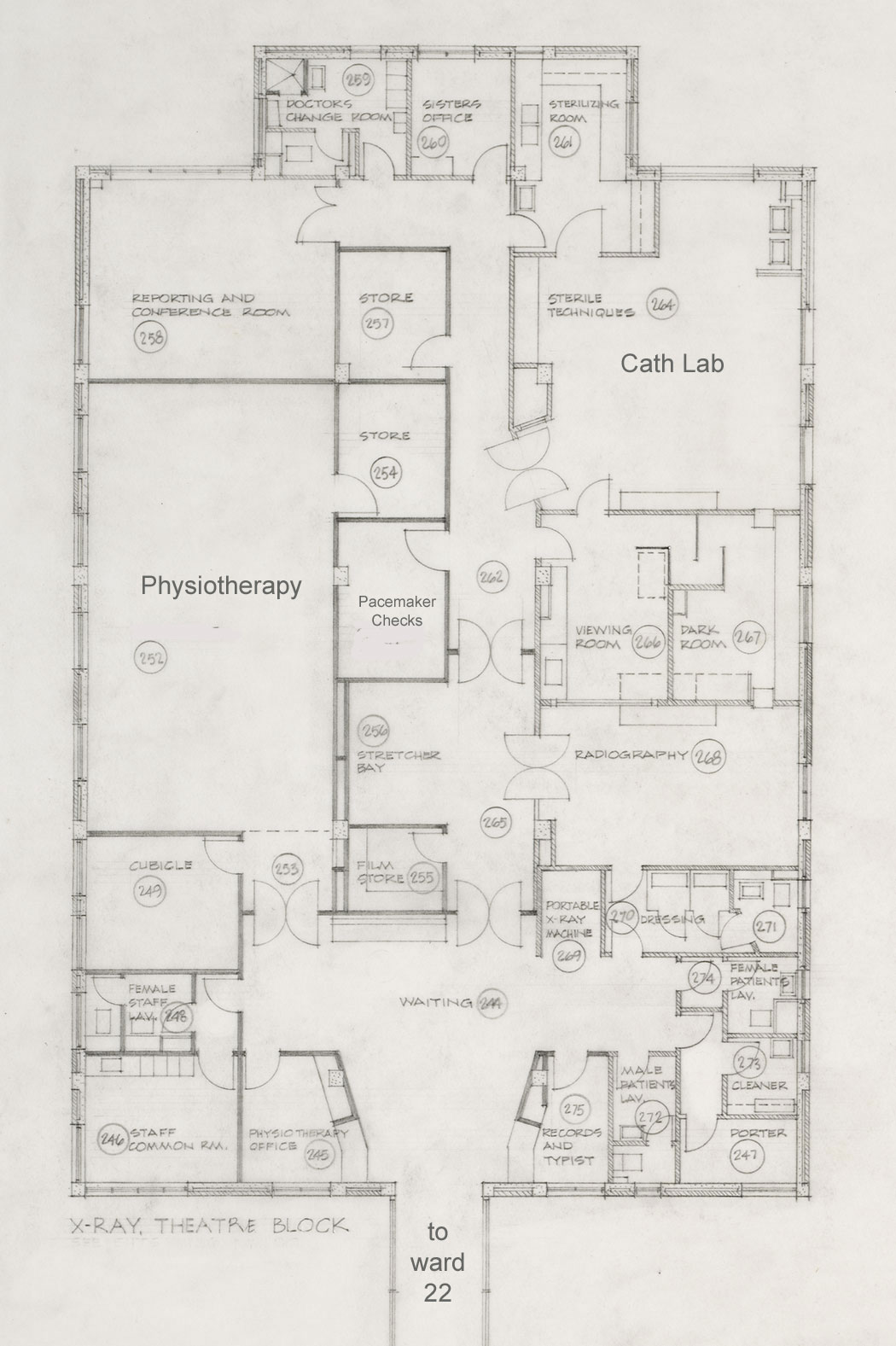 Seddon Cath Lab floor plan
Seddon Cath Lab floor plan
Weekly cardiosurgical conferences were held in the conference room at the back of the block.
This photo shows radiographer Ted Spiers demonstrating a patient set-up in the Seddon Cath Lab.
Beloe are technicians Anthea Denning-Kemp and Frances Stewart, Ron Easthope and Sister Bobby Morgan (both scrubbed) and radiographer Ted Spiers during a procedure in 1976.
 This cath lab served Cardiology's needs for the next seventeen years.
This cath lab served Cardiology's needs for the next seventeen years.
With a decision made to demolish the Seddon Block, the cath lab moved again in 1983, this time to the second floor of Radiology Services in the Clinical Support Block.
Cath Lab location 1983 - 2000
 Initially there was just one Cath Lab, designated Room N. During the 1990s, Peter Leslie mounted a major effort to secure a second Cath Lab (Room O), to allow emergency investigations and interventions without disrupting scheduled studies, and to provide a facility for pacemaker implants and electrophysiologic studies. In addition Peter pushed for making the new Cath Lab suite filmless with digital recording and archiving.
Initially there was just one Cath Lab, designated Room N. During the 1990s, Peter Leslie mounted a major effort to secure a second Cath Lab (Room O), to allow emergency investigations and interventions without disrupting scheduled studies, and to provide a facility for pacemaker implants and electrophysiologic studies. In addition Peter pushed for making the new Cath Lab suite filmless with digital recording and archiving.
The plans for the new suite are presented below:
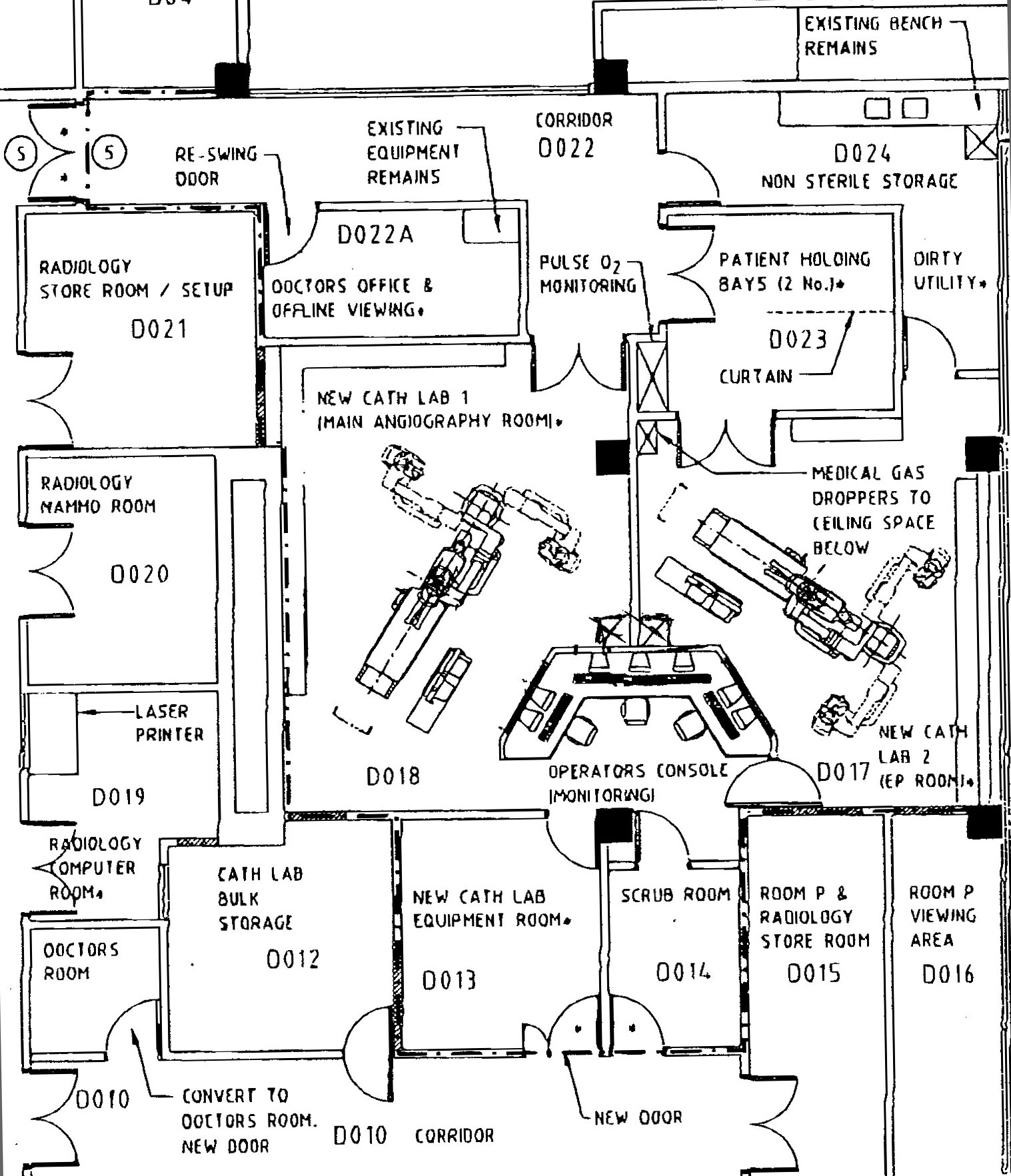 Room O ("new cath lab 2" above)was commissioned in 1999 along with digital upgrade of the radiographic equipment, and in recognition of Peter's role in achieving this advance, the Cath Lab Suite was named after him.
Room O ("new cath lab 2" above)was commissioned in 1999 along with digital upgrade of the radiographic equipment, and in recognition of Peter's role in achieving this advance, the Cath Lab Suite was named after him.
Toshiba equipment was installed in both rooms.
 View of Room O cath lab from shared control room.
View of Room O cath lab from shared control room.
 Charge Radiographer, Sharyn Armstrong in the control room.
Charge Radiographer, Sharyn Armstrong in the control room.
Room O was used for pacing implants as well as diagnostic catheterisations until 2003.
In 2003, Room O became the principle coronary intervention suite whilst Room N became the EP and Pacing Lab.
Cath Labs in the new Regional Hospital:
In the move to the new Regional Hospital, a third cath lab was commissioned, dedicated to EP studies, and ICD and pacing implants. Two other labs, (one seen in the photo), are used for diagnostic and interventional procedures.
 Elective patients are preassessed within the Cath Lab environment, and post-procedure they cared for in the same area also. These facilities are shared with other radiology investigation suites. There is a shared nursing and radiography staff across all radiology and cardiology investigation labs.
Elective patients are preassessed within the Cath Lab environment, and post-procedure they cared for in the same area also. These facilities are shared with other radiology investigation suites. There is a shared nursing and radiography staff across all radiology and cardiology investigation labs.
Cath Lab Staff
The early studies were done with help from senior radiographers and X-Ray department nursing staff, but without cardiology technicians.
Once Room E became the cardiac catheter laboratory, the Charge Radiographer was Robyn Harvey and the Charge Nurse was Sister Rae Parker. Robyn Harvey was replaced by Flo O'Sullivan in 1959, and Sister Parker by Bobby Morgan in 1961.
When the Cath Lab moved to the Seddon Wing in 1966, Ted Spiers was Charge Radiographer, assisted by Colin Butland and Barbara Collins, nee Clark. Later, David Ryrie replaced Colin and Barbara in 1977.
Bobby Morgan remained as Charge Nurse until 1977 when Margaret Vucetich suceeded her.
In 1983 the Cath Lab was now in Room N, CSB and June Carpenter was Charge Nurse. Mark Khull was Charge Radiographer from 1987 and Sharyn Armstrong from 1992.
Catherine Shaw became Charge Nurse in 1994.
When the new Regional Hospital opened in 2009, the nursing and radiography staff were shared across the Radiology special investigation area, and there was no longer a charge nurse or charge radiographer devoted to the Cath Lab.
Cath Lab equipment
The earliest investigations (14/12/1951 - 15/2/55) were done using saline manometry - pressures were expressed in cms of water, manually read from a tall saline-filled glass tube. Given that a pressure of 1mm Hg is equivalent to 13.3mm H2O, the tubing had be to be very tall if systemic or elevated right heart pressures were being recorded.
 A major advance was the purchase of a Sanborn two-channel recorder, above. This was first used on 22/3/1955.
A major advance was the purchase of a Sanborn two-channel recorder, above. This was first used on 22/3/1955.
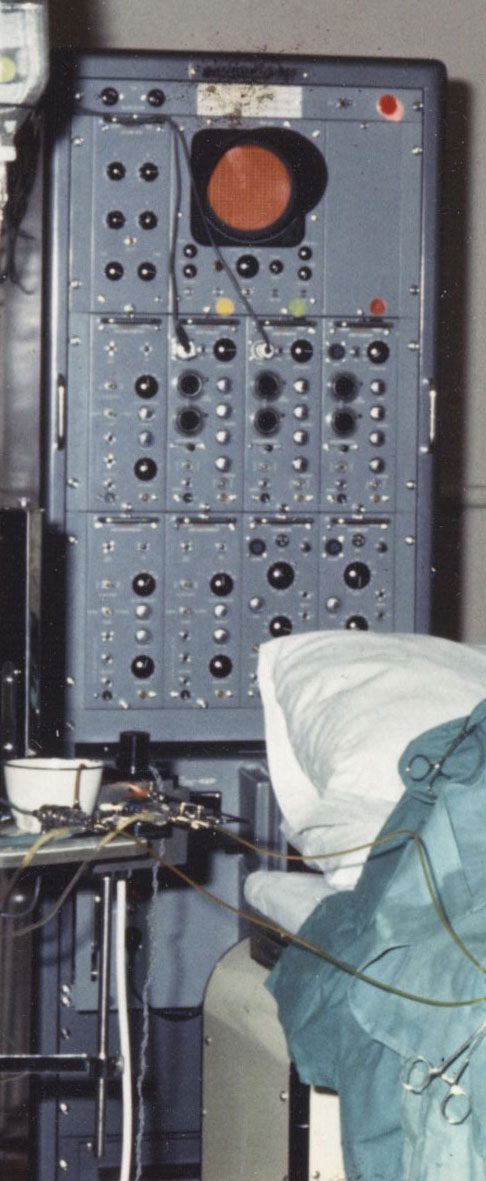
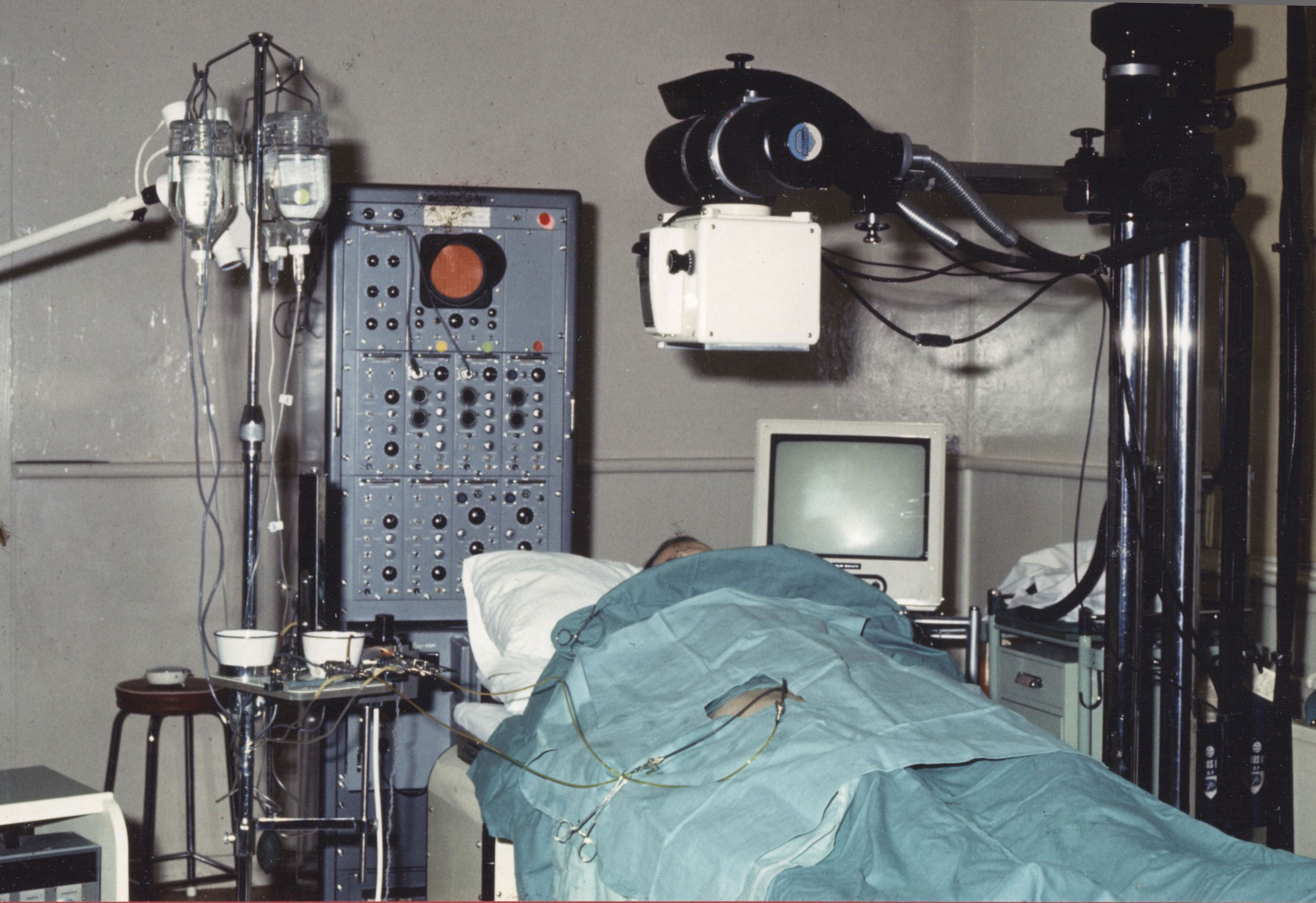
A multichannel recorder (later to become known as "Big Bertha") was used for the first time on 1/10/1963. This enabled simultaneous pressures from two or more sites, eg.aorta and LV in AS. Previously, the only way to assess severity of valve obstruction was by the recording of a single channel of pressure on withdrawal from LV to aorta.
Big Bertha served its purpose well for a good number of years. It used a photographic recording system for permanent record, which required processing in a dark-room.

The original pressure pre-amplifiers were constructed with valves, and from 1977 these were gradually replaced with solid state preamplifiers, and a larger monitoring screen replaced the tiny oscilloscope. The recording system was retained.
The photo shows the partial replacement of valved pre-amplifiers with smaller, solid-state ones.
One problem with Big Bertha, even in its modified state, was that the permanent record of pressures required photographic processing and was not available until after the end of a catheter procedure.
This was not critical for most diagnostic catheter studies but once electrophysiologic studies began, immediate inspection of hard copy records was essential.

The answer to this came in the form of a multichannel Honeywell recorder which had a direct print-out of recordings on wide format paper. In addition, it had an easily viewable large monitor screen.
It would be some years however before the department acquired the ability to freeze waveforms on the screen.
Big Bertha was still rolled out for use on occasions when service of the more modern recorders was required.

In time, the Honeywell recorder was replaced with a Gould 2000 machine which became known as "Sid". It would serve the Cath Lab well until the commissioning of the second Cath Lab (Room O) in 1999.
Now (1999), both Cath Labs were fitted with computer-based pressure acquisition systems. All catheters in use during a study were connected to pressure-monitoring lines at the catheter table, and although pressures were displayed on suspended monitors within the Cath Lab, any recordings required were run by a Cardiology Technician who was situated behind the lead glass screen bay, remote from any exposure to radiation.
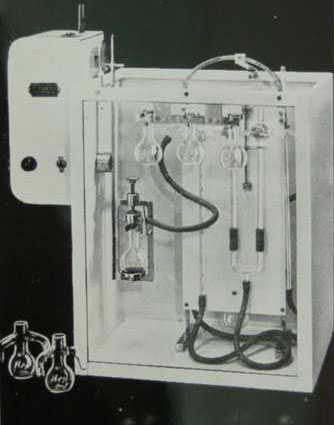
Throughout the 1950s, investigators were required to send blood sample to the Pathology Laboratory, where the senior biochemist, Hugh Olive, measured O2 saturation using a modified Van Slyk apparatus (shown in photo). Waiting for results to come through was always frustrating, and from time to time, repeat samples had to be sent to the Lab as the first samples had proved unsatisfactory - eg. clotted.

On 11/4/1961, the Kipp Oximeter was in use in the Cath Lab for the first time. Blood was withdrawn through a haemoreflector cuvette (seen left), which was connected to the oximeter (below). This still required selected duplicate samples to be sent to the Pathology Lab for calibration of the Kipp.

From the earliest catheter studies done, measurement of cardiac output (if required) was based on the Fick principle. This required knowledge of the AV oxygen difference (readily measureable), and timed oxygen consumption which was not so easy to obtain. In the early years, oxygen consumption was calculated by using the Metabulator. One of these devices had been acquired by Fred Bowerbank in 1926 for measurement of BMR. A similar model was in use in the cath lab in the 1960s (see below).

From the 1970s, occasional use of a Douglas Bag collection of expired air was used to calculate oxygen consumption. Typically the bag was brought to the procedure by Julia Ripley from the respiratory lab where the gas analysis was subsequently done.
From the 1980s, thermodilution techniques were used with the equipment below.

As coronary disease became the dominant reason for cardiac catheterisation, cardiac output calculations were required much less often, but were still deemed helpful for calculation of pulmonary vascular resistance in patients with pulmonary hypertension.
Radiographic and EP equipment are detailed elsewhere.
Cath Lab Screening and Angiography
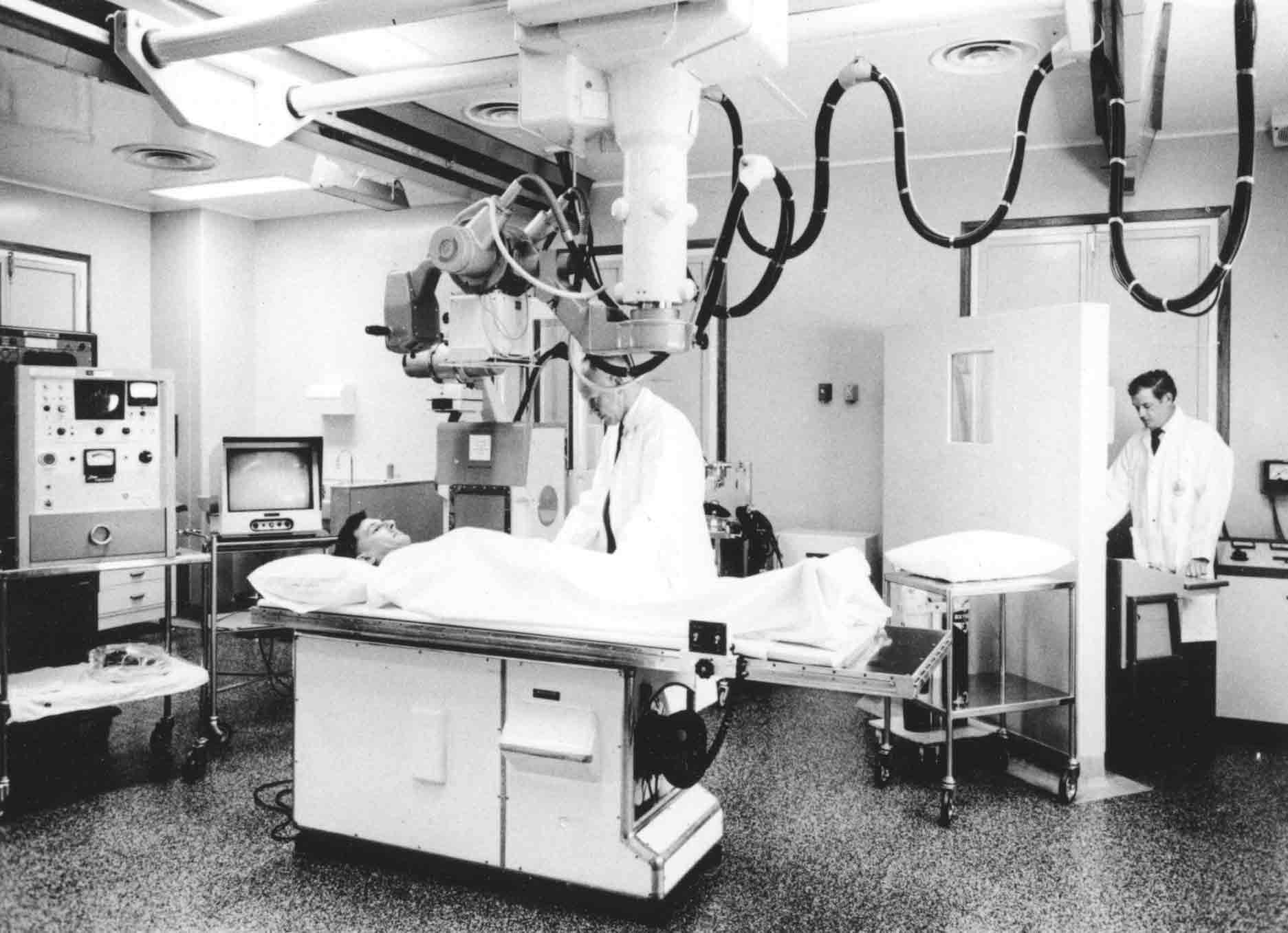
Until 1963, procedures were done in a darkened room, requiring all cath lab personnel to dark adapt using infrared glasses. Screening was achieved with a horizontally aligned viewing screen situated over the patient's chest, which meant that only those directly involved could see the non-intensified image.
I remember very well the occasion when, as a house physician, I was privileged to be able to attend a cardiac catheterisation session. I was duly given a pair of infra-red glasses to wear, and despite getting as close to the action as I could, I was unable to see a thing. No one told me that the glasses weren't intended for wearing throughout the procedure!
In 1963, the first television screening system with image intensification was installed in Room E, allowing all procedures to be performed in a normally lighted room.
The first angiograms (venous injections of contrast) were recorded using a modified Fairchild aerial mapping camera.
From 1955, angiograms were recorded using 'cut films', which required manual pulling of multiple unexposed films into position every 2 - 5 seconds to capture images of the transiting contrast.
When I was a medical student, working in varsity holidays as an X-Ray porter, I was allowed to watch an angiogram being undertaken in the main X-Ray department. Standing alongside one wall of the room, I was concerned that a mattress lying on the floor nearby was in the way of staff moving about. Having removed the said mattress out of the way, I was severely rebuked by Roy Sample, Charge Radiographer, as the mattress had been in the correct position to cushion the exposed films as each was pulled from under the patient!

An automatic 14x14 film changer, similar to the one shown, was installed in 1958. This allowed for exposures to occur at six frames / second.
The first selective (RV) angiogram was performed one year later in 1959
In 1963, along with the Cinelix image intensifier and television viewing, cineangiography was introduced. The 35mm film was processed in the standard X-Ray processor, and sent to the National Film Unit in Miramar for copying into 16mm format, so that it was suitable for viewing using the available projectors of that time.

The next advance occurred with the opening of the Seddon Cath Lab. Biplane roll-film angiography was now possible.
This photo shows Dr Alistair Wilson viewing a roll-film angio with radiographer Ted Spiers.
Note the loop of 16mm cine film hanging on the viewing screen.
Selective coronary angiography was first undertaken in 1969. Around this time, a Targe Arno 35mm projector was acquired, removing the need for National Film Unit processing. A Phillips Plumbicom system was installed in 1972, with improved cine facilities including videotape, and a patient cradle was attached over the table to enable patient rotation to any desired angle.
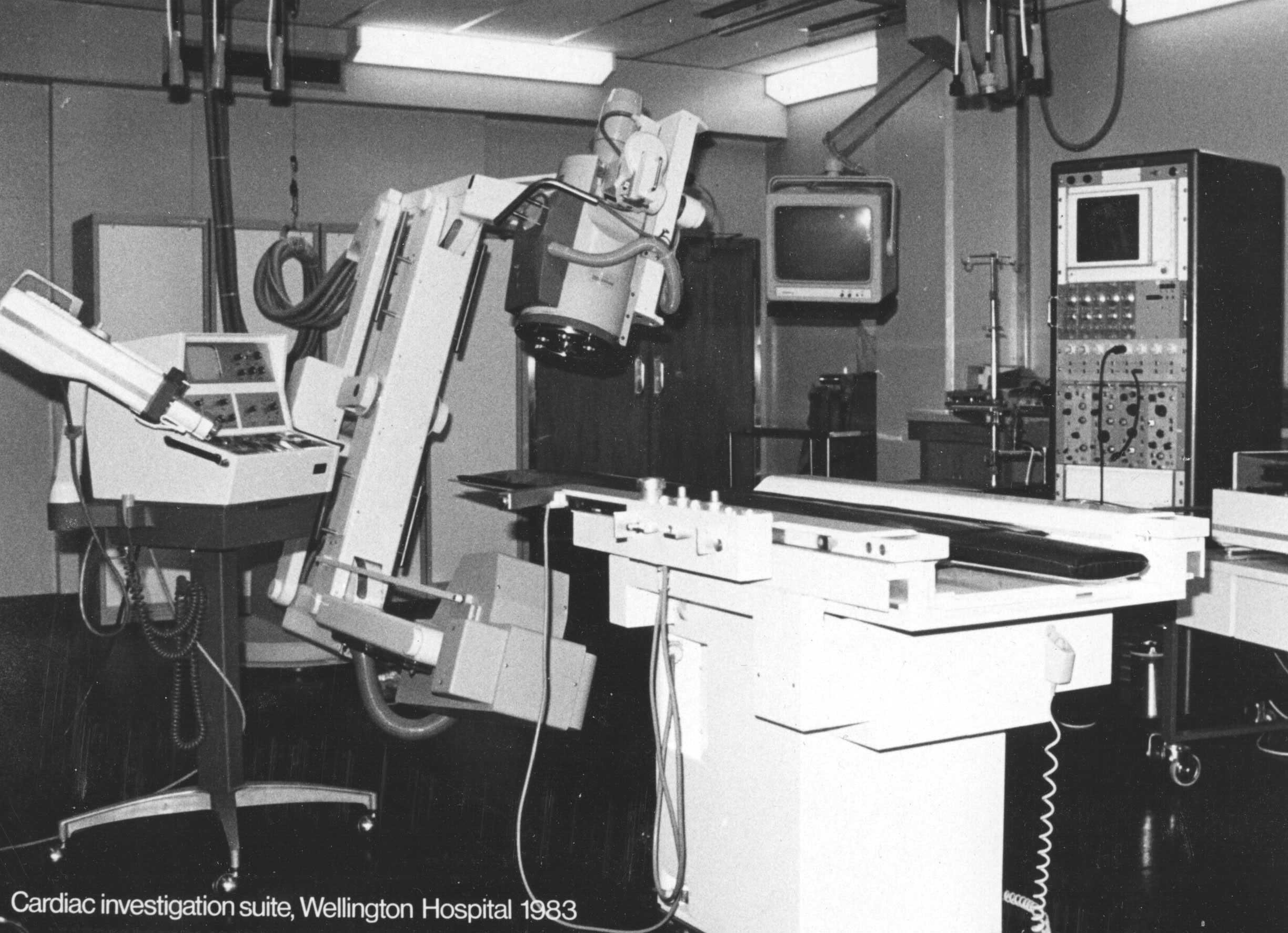
In 1983, with the move to Room N, CSB, a Phillips C-arm screening system was in place, making the patient cradle obsolete.
In 1999, a two room Cath Lab suite was commissioned, with Toshiba filmless equipment.