Mildred Gertrude Rees
b. 1869 d. 21/8/57
(At the time of the Wellington Hospital Centennial Celebrations in 1947, Mildred Rees who trained as a nurse at the hospital 1891 - 1894 was interviewed, the proceedings of which were published in an unidentified newspaper clipping now located in the CCDHB archives, Archives NZ)
1891
"All these memories bring a chuckle to jovial Miss Rees of Nelson"
When Mildred Rees entered the hospital as a probationer in 1891 it was a tiny institution, boasting only one resident medical man, Dr John Ewart, and some 30 nurses. She recalls that the first six months work brought her exactly £3, and that after three years she was receiving the unbelievable sum of £26 per annum for her services. That their work was a labour of love to these nurses is emphasised by such conditions. Apart from annual leave of two weeks a year, a day off-duty was quite unknown.
Although the eight-hour day for nurses had just been introduced, theirs was a seven-day week and much overtime went unpaid. A trip into town meant boarding one of the horse-trams that plied along Adelaide Road in those days of naked gas-lights and hansom-cabs, and if she had not a late pass in her bag woe betide the nurse who was out after 10pm! These much-coveted permits were issued once only a fortnight. However, despite formidable uniforms, hard work and rigid discipline, the nurses were a happy family.
Miss Rees tells that, on joining the hospital, she was quartered with three other probationers in a bedroom along-side the morgue since then, as now, accommodation was cramped. Often the nurse would be awakened by the midnight arrival of another occupant next door. As there was no hot water in this part of the building, each day began with a cold bath for these Spartans.
Edna Pengelly
b. 1874 d. 1959
(extract from “Nursing in Peace and War”, by Edna Pengelly. - courtesy NZNO Library)
1st January, 1904
So began my first day in Wellington Public Hospital. In those days we provided our own blue uniform, later to be those of the hospital, with a change of colour to grey. For three months we struggles with our home-made “blueys”, providing our collars, cuffs and aprons. I may say in passing that the collars were murderous things, almost cutting our throats. The cuffs fortunately were removed while we washed, polished and scrubbed. During those first three months, the new probationer wondered anxiously whether or not she would be kept on. If so, she would change the colour of her uniform to pink, being called a “pink” nurse for some time, during which she would be taking greater responsibility and learning much.
We rose at 5 a.m., on duty at 6 a.m. This was in order to base the duties on an eight-hour period – three eight-hour periods in the 24 hours.
Lizzie Ida Grace Willis
b. 1881. D. 1968
(extract from “A Nurse Remembers”, by L Ida G Willis. - courtesy NZNO Library)
January 1907
I began my training in the Wellington Hospital under the Matron, Miss Frances Keith Payne and the Medical Superintendent, Dr John Ewart. Fifty-eight years ago there were no preliminary training schools for nurses. Raw recruits, as we were, it was straight into the wards for us – a real ordeal for shy, inexperienced girls.
The hospital main buildings consisted of six wards of 25 beds (supplemented with stretchers) and a side room of two beds, a kitchen with gas ring where sterilization was done between two basins. (The sterilizer came later.). The bathrooms and toilets were at the end of each ward and were called “the backs”. Behind the main building were the Children’s Wards, isolation block, and a large two-storied building for the aged men and women. Shelters on the hillside were for tubercular cases. There were about six shelters, some with two beds and some with four.
The Nurses’ Home (just completed) was three storeys, with single rooms. We were very lucky, for prior to this the nurses slept in cubicles above Ward 5. There was a maid to each ward and she attended to the corridors and washed and polished the floors, and looked after the fireplaces. She also helped with the patients’ meals and washed up.
The nurses were called at 5 a.m. and reported in the ward kitchens for a compulsory cup of tea and to read the night report. On duty in the ward at 6 a.m. Each junior nurse took a side, to take temperatures, make beds, give out washes to patients who could wash themselves. Then swept and dusted.
Occupationsfor women were very limited. Many employers were still horrified at the idea of women in their offices. Even in hospitals the entrants had to be at least twenty-three years of age so that they began their work with a more realistic acceptance of the conditions. Dr. John Ewart, the Medical Superintendent and Miss Payne, the Matron, were people of the finest caliber. From them we received the best of training in every aspect of our profession. They never failed to stress that the care of the patient must come first. I can say here that this fundamental part of our training so deeply implanted by these two wise, devoted teachers and guides proved itself in later years. During the First World War, when New Zealand’s Sisters were seconded to the Imperial Army Nursing Service in England, Egypt, France or on Transport or Hospital ship duty it was a tribute to such training that the Chief Matron and other Matrons were reluctant to part with them.
But that was still to come and meantime we were learning under the supervision of the Sisters, wise upright women and firm disciplinarians, imbued with the purpose of turning out efficient, dependable nurses. I look back with gratitude and admiration to those women who demanded nothing less than perfection from us and were friends for life. We owe something to the patients, too, who sensed the near panic and bewilderment of the young probationers, fresh off the grass, and finding themselves in a highly disciplined, highly organized world, so different from that they had just left. They helped to lighten our ignorance with hints and advice in their own quiet sympathetic ways. Of course it was hard work. We had a seven-day week; an eight-hour day, which in special cases became twelve hours; three weeks holiday and a late pass to 11 p.m. once in three months. Occasionally, on change of duty, there could be an all-night pass. One was on day duty for three months, and for the same period on night duty. As for payment, this seems to have had little relation to the hours worked or the physical labour entailed. For the first three months we received no payment, but after that 5/- a week and a slight rise in the second and third years.
Our uniforms or appearance could not compare with present-day wear, as the hospital had no money. But how proud we were to wear the patched, faded, lengthened uniforms showing where tucks, etc., had been let down, and only our aprons, cuffs and collars provided by ourselves were new………
……At the end of three years, having passed the Hospital and State Examinations, I was appointed Sister of Ward 1 and later Night Charge Sister at £70 per annum. A strenuous but exceedingly interesting duty……
Ellen Iris Schaw
b. 1882. d. 1970. source: Wellington Hospital nursing archives
1907 - 1910

Iris recorded some recollections here
Marie I Farquhar
b. 6 June 1905. d. 1990
(from “It Just Goes to Show”, by Marie Immaculee Farquhar Cleland, 1970. - courtesy CCDHB archives, Archives NZ)
1925
August 15th, 1925, was the day when Sister Clarke’s lectures began for me.
Lecture 1
To Strip a Bed. To Make a Bed. To Make an Operation Bed.
To Give a Bed-bath. Bath temperatures.
How to give a Patient a Bed-bath.
Procedure, Sponging, etc.
August 29th Lecture 2
Poultices and Fomentations
Linseed, Antiphlogistin, Mustard Leaf, Mustard Plaster, Bread Poultice, Starch Poultice
September 5th Lecture 3
Counter-irritants, continued:
Turpentine Stupe
Opium or Belladonna Stupe
Breast Fomentations, temperatures, by mouth, axilla or rectum.
Pulse rates, Tachycardia, Irregular, Intermittent, Dicrotic.
Respiration, Dyspnoea. Cyanosis, Orthopnoea, Cheyne-Stokes, and Apnoea.
Lecture 5
Enema, Procedure, etc.
Lecture 6
Rectal Salines, Procedure, etc
Care of Rubber Appliances
Bedsores and Causes
Injections
Classification of Drugs and their effects
Administration of Drugs
Fluid Measures, and symbols.
These lectures and demonstrations were very interesting. But some things were left unexplained. For instance, a new probationer having learnt the correct temperature for hot-water bottles, took from her pocket her clinical thermometer (a good one - - the gift of her father) and proceeded to test the hot-water bottle. She came to me in tears because she broke her thermometer. So, “a little knowledge is a dangerous thing.” Most nurses learnt the hard way – trial and error.
The Medical Superintendent
 Dr Macdonald Wilson, Medical Superintendent of Wellington Hospital, was known by his nursing staff as “Father”. This, in true sense, a term of endearment to nurses reporting sick; but perhaps to Staff Nurses tinged with a degree of awe or fear when suddenly Dr Wilson would appear in the Ward.
Dr Macdonald Wilson, Medical Superintendent of Wellington Hospital, was known by his nursing staff as “Father”. This, in true sense, a term of endearment to nurses reporting sick; but perhaps to Staff Nurses tinged with a degree of awe or fear when suddenly Dr Wilson would appear in the Ward.
Seniors said, “You won’t really know “Father” till you’ve seen him in the operating theatre!” Later, I understood – forceps failing to grip, would go flying across the theatre floor (to be disposed of to some less-important Ward Trolley). But, such display of impatience genuinely built up confidence in Dr Wilson’s efficiency.
Juniors and Seniors all thought a ‘lot’ of “Father”. He was attentive to the sick nurses. They were treated with respect and concern. With a staff little over two hundred, Dr Wilson had real problems. The state of health of the general public – and the nursing staff, to cope with overflowing wards, was no small responsibility. And during 1925 – Dec 1928 it seemed that not only did beds line the walls, but stretchers were set up ‘head-to-tail’ right down almost every ward in Hospital – even Ward 4, Fracture Ward. As motor cars and motor cycles increased in popularity, so did the accidents fill Ward 4. Nurses were overworked. They could not get leave days – they could not even get off duty on time, because of the length of dressings or 2hourly treatments which were required to be done by one senior nurse in each ward. Sick nurses so depleted the ranks, the well ones were ‘flattened’ by fatigue. Several developed T.B. Many resigned. Working sometimes as long as six weeks, seven days a week, could bring the strongest to breaking point, which one day’s leave could not restore.
Sick nurses were never forced back to the wards, but first were put on trial in what was known as ‘the Working Room’ with Miss Lampp, Sub-Matron in charge. Here they were given a few hours work each day – even be it ironing shrouds! ! ! ……..
…… Dr Macdonald Wilson was thorough in his examination of all nurses reported sick, nor ever gave the impression that any was ‘swinging-the-lead’.
There was sincere regret when he resigned his position as Medical Superintendent, Wellington Hospital.
Joan Frances MacKenzie-Boyle
b. 18/12/1914. d. 2007
(personal communication in 2006 from Joan Frances MacKenzie Loeber nee Boyle)
1934
At the age of 19, Joan went for an interview with the Matron, Miss Cookson, having got the idea of a career in nursing around six months earlier. She was accepted for training and presented herself at the hospital on 2/1/1934.
“There, we met the Tutor Sister, Sister Tomlinson, and I don’t know why but in those days the sisters all seemed to be tall and elegant and really rather beautiful because they wore the most attractive uniforms; sapphire blue uniforms with long sleeves, white starched cuffs, a stiffly starched white collar and their big white organdie veils; a most becoming uniform and one which almost demanded respect. Sister Tomlinson talked to us about what to expect, to stand to attention with your hands behind your back to your seniors, a strict but not restrictive standard of etiquette was demanded of us and good manners. And then we went back to the home and we got dressed, she showed us how to make up our caps and then off we went. We were terrified; I was petrified! Didn’t know what to expect, I had never been in hospital, I had never seen anyone sick. I began to wonder what I had done. However, you were kept so busy, there was something happening all the time, you didn’t have time really to worry, you were just there to do what you were told. That was my reaction. We were taught the basic skills of nursing. Bed making; making up a bed for an operation bed. We learnt to sponge patients, take temperatures, pulses. There were no sophisticated diagnostic aids in those days. And these things and learning to be observant were all we had. We had to learn them well and we did. We had a model in a bed, we all had to sponge that model. We learnt to give enemas, and to do all kind of things; we learned to test urines.
Preliminary School classes were held in the mornings and in the afternoons we were sent to the wards. There were two probationers to each ward. I was first sent to Ward 1, the women’s surgical ward. I was very naïve. There were seven women there because of illegal abortions, some self-performed.”
Grace Augusta Brandon
b. 2/2/1912. d. 22/8/2004
(from the Wellington Hospital Nursing Journal, 1934)
1934
A Few Thoughts on Nursing from my First Year’s Training
The Opportunity
I am given the opportunity of training in a profession, which requires the greatest skill, and is endless in all that it can teach.
Personal Development
By starting at a humble beginning, I learn to stand back, and learn from others, and remember that I am only one of many, and yet my job is all important to the whole.
Contact with the People
I discover that there is a good and brave heart, and clean soul under many a rough surface, and indescribable darkness in others.
Co-operation
By working with a common will, and with my fellows, I find friendships, and my job better done.
Care of the Aged
Nurses are the whole life and interest of those chronic cases who are helpless and friendless, and their lives are what nurses make them. I have heard it said that nursing is a practical touch of religion.
Kathleen Moynihan
b. 1911. d. 1992 from 'Wellington Hospital Educating Nurses for more than a century", by A. L. McDonald and C. Tulloch

1932
Our class of eleven only, plus one entering in May 1932, was the first intake for six months, possibly owing to the economic depression. We were the only students wearing pink uniforms. We had no preliminary course and there was no tutorial staff. Lectures were given by senior and junior medical staff, the Matron (Miss Cookson), and occasionally a nursing procedure was demonstrated by a ward sister - on "Dolly Chase" of course - no patients were used. All other learning was acquired in wards by practical experience.
Promotion exams were held every six months. There were no State exams until final registration. For the first year we were known as probationers ('pros' in colloquial language). At the end of the year, following success in passing an exam in anatomy and physiology, plus satisfactory ward reports, we were "signed on" for training.
Ours (1932-35) was the first class to have a Graduation ceremony, only because we suggested it. We paid for our own medals which were sent to us in 'Craven A' cigarette tins and which we handed in to the Matron's office so that they would be well and truly pinned on by the Chairman of the Board.
This first ceremony was held in the Senior Nurses' sitting room in the old Nurses' Home.
We had no study days or block system. Lectures were given at times to suit the lecturer. Those on duty had to return to their wards afterwards to make up the hour of absence from the ward. Those off duty were expected to attend all lectures."
Elizabeth Anne Gell (Betty)
(source Wellington Hospital nursing archives)
b. 13/4/1915 d. 2003
1934
Betty Gell, who trained at Wellington Hospital and went on to be on staff for 45 years, recorded her recollections here
Dorothy Mae Carson, nee Hamlin
b. 28/5/1923. (personal communication)
1941
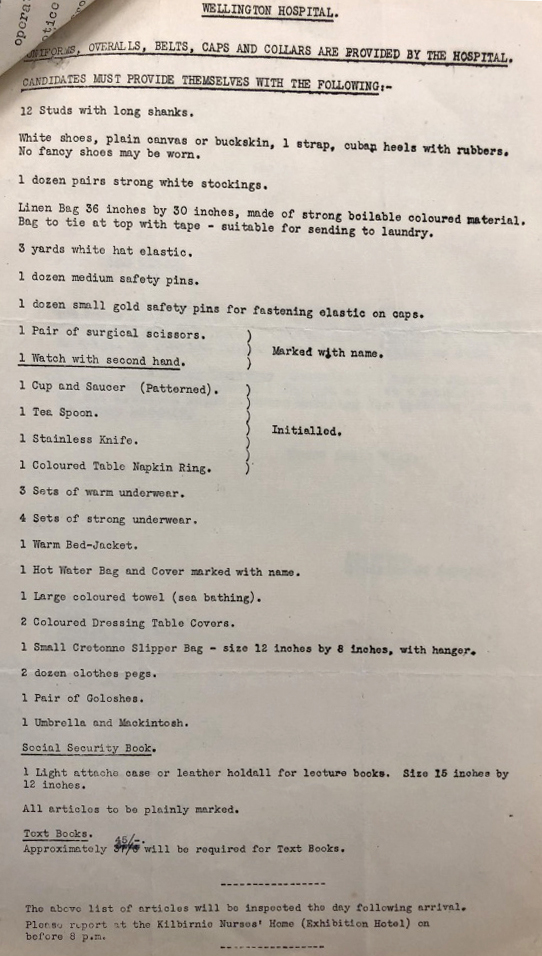
Presented to the Kilbirnie Nurses' Home in July 1941 aged 18, having received the list of requirements below. She was surprised to learn that she had to pay for all items and had to borrow money to be able to comply. Remained in the Kilbirnie Home until Preliminary School completed. Preliminary School tutors were Sisters Scott and Stone. 
Then moved into the main Nurses' Home (No. 1) . Recalls studying on the Home veranda with fellow students in the summer months.
A lot was expected of student nurses. In wards, providing bed pans, sweeping floors with tea-leaves. If anyone more senior came into ward, required to have hands behind backs. It was in the wards that she made friends with fellow student nurses.
She remembers the heavy wooden screens that nurses had to pull around patients’ beds for privacy – a devil of a job for a nurse on her own, as there were always three screens that had to be manoeuvred. Mae also remembers an incident getting to the end of a night shift and taking the trolley with trays of notes and medical items back to the ward office. The entrance to the office had a bit of lip to it and negotiating it was always tricky for a young nurse. A patient saw her struggling with it and offered to help, but he ended up pushing the trays off the trolley, breaking several thermometers. Mae was called to the matron’s office and told she had to pay for them all. It seemed a lot of money then, and very unfair because it wasn’t her fault. The matron, however, suggested Mae was flirting with the patient and she would hear nothing of her protests!
Joyce Martha Irving, nee Stanley
b. 9/12/1923.
(extract from "Class of 42" by Joyce Irving and originally published in the magazine Memories. Reproduced here with the permission of the Editor)
1942
On 4 February 1942 we assembled at the Nurses Home, Kilbirnie to commence our nursing training at Wellington Hospital. The Nurses’ Home was previously the Exhibition Hotel built for the 1940 Wellington Exhibition and now used for new intakes of student nurses. We travelled by tram each day from Kilbirnie to the Prelim School at Wellington Hospital. Our Tutor Sisters were Sister Scott, who taught Anatomy and Physiology from a book written by Drs. Gowland and Cairney, and Sister Stone who taught the Techniques and Practice of nursing.
During the later stages of Prelim School we started going into the wards each day for practical experience, such as making and changing bed linen with the patient still in bed, making sure that the corners were all mitred correctly as Sister Stone watched with an eagle eye, sponging and giving back treatments for the prevention of bed sores, and mastering the art of bed pans, which required two sets of screens to be placed around the bed. These were heavy to haul around the ward.
We were taught how to sterilize and set up treatment trays, the right instruments in the correct order for specific treatments. The wards were large with rows of beds down each side and frequently extra beds down the centre. The floors were kept highly polished, but the junior nurse had to sweep first, sprinkling cold damp tea leaves scattered about, to collect the dust. I was always being told to hurry. I would just get the tea leaves scattered and start sweeping when the patients called for bed pans. I found it quite a dilemma, the Doctors would arrive for their morning rounds, walking through tea leaves to find their patients behind the screens – no wonder the Sister growled at me, but with practice I did get faster.
Towards the end of Prelim School we were to watch an autopsy. Nurses with surnames A to M went first, the rest of us to go the next day. So many nurses fainted on the first day that the second day was called off.
When the two months of Prelim School came to an end and we had passed our exams, we started duty in the wards. We went in pairs and my first ward was men’s Urological. With freshly starched uniforms we arrived early and with eager anticipation to meet the ward Sister, to be shown around and to have the duty lists explained to us. Outside the Sister’s office and before we entered the ward, the Sister pointed to some rooms across the passage, and in a hushed voice told us “These are for V.D. patients, attended to by orderlies, and nurses don’t go into that area”. We didn’t need telling twice. As a couple of naïve 18 year olds we thought V.D. was on a par with the Plague and kept our distance.
The war news was getting very grim….. For safety reasons the Wellington Hospital Board decided to move the bed-ridden elderly patients from the Victoria wards to Otaki Children’s Health Camp. I was in the first group of nurses to travel by train to Otaki to prepare for their arrival. The patients arrived in convoy; by private cars and ambulances. The health camp was a large airy building but very cold and draughty, altogether not very suitable for the old and frail, some of whom hadn’t been out of bed for years, most suffering “senile decay” as it was called then and quite a number died soon after the shift. The nurses lived near-by in the Capital Guest House at Otaki Beach, complete with an outside loo. We enjoyed the occasional swim, although Otaki Beach was unsafe and several drownings had been reported about that time. During my second turn of duty at Otaki I did night duty.
A time was spent at Ewart, a Hospital for TB patients. My first duty in the morning was emptying the white enamel mugs of bloodstained, highly infectious sputum. I used to feel physically sick, so enough said about TB nursing. The Nurses’ Home at Ewart Hospital was a very elegant two-story home, originally built for the resident doctor. Coming off duty we would sit by a log fire and drink hot cocoa and listen to the request session on the radio.
Fever Hospital, further up the hill from Ewart, was my next assignment. Mt Victoria was a frightening place following a recent murder, so we never ventured out alone. Fever Hospital had some very sick children with scarlet fever and diphtheria and an outbreak of chicken pox. Coming off duty we had to take a Lysol bath, even so some of the nurses caught scarlet fever; we had been vaccinated for diphtheria. There was a nurses’ Sick room at the main Hospital, but they didn’t take infectious diseases, so we cared for our sick nurses as best we could and tried to make life as comfortable as possible for them.
Wards 21 and 22 were being prepared for the arrival of the first hospital ship from the Middle East, soldiers from the Greece and Crete campaigns. These wards were a more recent addition to Wellington Hospital, six beds to a room with sliding curtains, making nursing easier.
As a junior nurse in a surgical ward, I remember sitting with patients as they recovered from anaesthetic. Patients came straight from theatre after surgery back to the ward, and had to be watched carefully until they regained consciousness. The ward sister would keep popping around the screen to check and gently pat the patient’s face with “can you hear me Mrs Smith, time to wake up”. Gradually the eyelids would flicker and a few gurgling sounds and you were aware they were coming around. Lying in an enamel tray by the bed was a pair of tongue forceps, to be used we were told ‘if the patient turned blue and swallowed their tongue’. Wounds were dressed and stitches removed and junior nurses were encouraged to observe and assist where possible. Patients were nursed in bed for at least ten days following surgery.
Ngaire Gwynne Nicol, nee Teasdel
b. 18/8/31 d. 19/12/2000
( reminiscences of her days as a student nurse, courtesy CCDHB archives, Archives NZ)
1949
Junior NurseOn September 9th, 1949, my Prelim Class went into Nurses’ Home No. 2, the first to do so. For the previous few years, the new classes had been going into the old Exhibition Hotel at Kilbirnie. Junior Surgery Class came over from Kilbirnie Home and moved on to the second floor of Home 2 and they and the previous Prelim Class were there to welcome my class of 32 on to Floor 3.
The Home Sister, Sister Rowlatt, padded down the long corridor opening doors, calling names and never ceasing to expound the rules - Nurse Teasdel Room 32, see that your lights are out at 9 p.m., no one in the bathrooms after 8.30, there will be a room inspection on Wednesday, you must be dressed and up to the Main Home for breakfast at 7 a.m. and so on and so on. We were so regimented, so restricted, it is unbelievable to think back and remember how we not only accepted it, we expected it. I remember a night sister banging on a bathroom door at 9 p.m. one night and yelling “Get out of that bath! You’ll never get the Gold Medal”.
At the end of a week one girl escaped down the fire escape one night and never returned – the fire escape being the only way out – the girl was so terrified of the system. It was an era of utmost obedience and respect and nurses who did not comply with regulations created scandals.
We cleaned with damp paper, tea leaves and Turk’s Head Brooms. We hand washed, boiled, dried and folded masks. We cut, folded, packed gauze swabs. We rolled cotton wool balls. We mopped under the beds when concluding a sponge. We made tow pads. We cleaned enamelware. We held capes over our arms and spoke to seniors with eyes cast down. In the dining room pinks did not sit with mauves, nor mauves with staff nurses. We sat where the dining room supervisor directed us.
After Preliminary School my first ward was 24 with Sister Pederson and Staff Nurse Kath McDonald. This was in the new surgical block – general surgery – the ward honorary being Joey Pullar, resident surgeon. I was very lucky to start with such a gentle and understanding ward sister. I began work on the day of the State Final Exams. What an experience it was to sit finals in those days. All senior nurses lived in Home One and, of course, there were no married students or anyone living out. You stayed single and you stayed in.
On the morning of the first paper the seniors would leave their rooms immaculate and unlocked. While they were away the ward or department in which they were working took over the decoration of the bedroom. It was quite an occasion as the staff competed with each other to give their girl the best room. Streamers, balloons, flowers, parcels, cakes and food galore. The windows were painted and sported messages such as BEST OF LUCK MARGARET. Looking at the home as you walked up the drive, well, it looked just like Christmas and, at 12.30 when the students came back after three grueling hours of Medical Paper, there were corridors of fairyland. No matter how terrible you felt, it was a jubilant “surprise” to see your room. An emotional experience and climax to three years of hard work.
Then, in keeping with tradition (nothing over 2/6d) were the gifts from each other. The girls moved from room to room admiring each others decorations and surreptitiously slipping their own gift – one to each bed. By the end of the day maybe fifty parcels, all gaily gift wrapped, from classmates and friends. In the evening all those with family near held court and visitors toured the corridors to see the displays. They were wonderful times and great was the laughter and the tears.
Well, here I was in Ward 24 with Sister Pederson and she said “Now you come with me. We are going to decorate our room for our nurse”. I helped her in the ward kitchen with Julie the Irish kitchenmaid. We made mice out of prunes, licquorice straps and jelly beans, among other things. We went up to the Home and decorated it with all sorts of things out of a box from Ward 24 store room which was marked in big black letters “STATE DECORATIONS”. Sister Pederson said to me “I suppose, Nurse Teasdel, you think that your time will never come, but it will”. And it did. I always wished I had been in 24 to have her do my room but it wasn’t to be. She had left before I had finished my training.