The first deep vein thrombosis (DVT) thrombectomy procedure in the North Island using the new INARI Medical ClotTreiver device was recently performed at Wellington Regional Hospital by the Interventional Radiology and Vascular Department. This new device can remove all the clots in a single procedure without the use of clot busting medication.
The introduction of this new ClotTriever device, produced by INARI Medical, is a game changer for the removal of blood clots according to Dr Shueh Hao Lim, Interventional Radiologist at Wellington Regional Hospital. He was the main operator during the first use of the device, and he talked us through the procedure and how the device will not only benefit patients, but the hospital as a whole.
DVT is a condition characterised by the formation of blood clots within deep veins. Traditionally, the treatment for DVT has mainly involved anticoagulation therapy. This therapy aims at thinning the blood with the hope that the clots dissolve on their own. Recent advancements in technology have revolutionised the approach to treating DVT. These advancements offer patients more effective and a less invasive solution, with the main aim of reducing post thrombotic syndrome in the long term.
The first use of this device in New Zealand was in Christchurch earlier this year. Dr Lim and his team have done one procedure so far, but are keen to find other patients who would benefit from this.
“They’re not elective, so they come in as an emergency. You never know when someone develops a clot and when they come in, we have a window of roughly a month but ideally the first 2 weeks to treat, because if you wait longer, the clot starts to solidify. With the INARI ClotTriever device, we can now treat clots that are slightly older with minimal risk,” said Dr Lim
“We first used the new device on a patient who presented to our vascular department with left leg swelling, pain and difficulty mobilizing. They had an ultrasound in the community, which showed extensive clots going from just above the knee up to their iliac veins. This was confirmed by CT scan on arrival,” said Dr Lim.
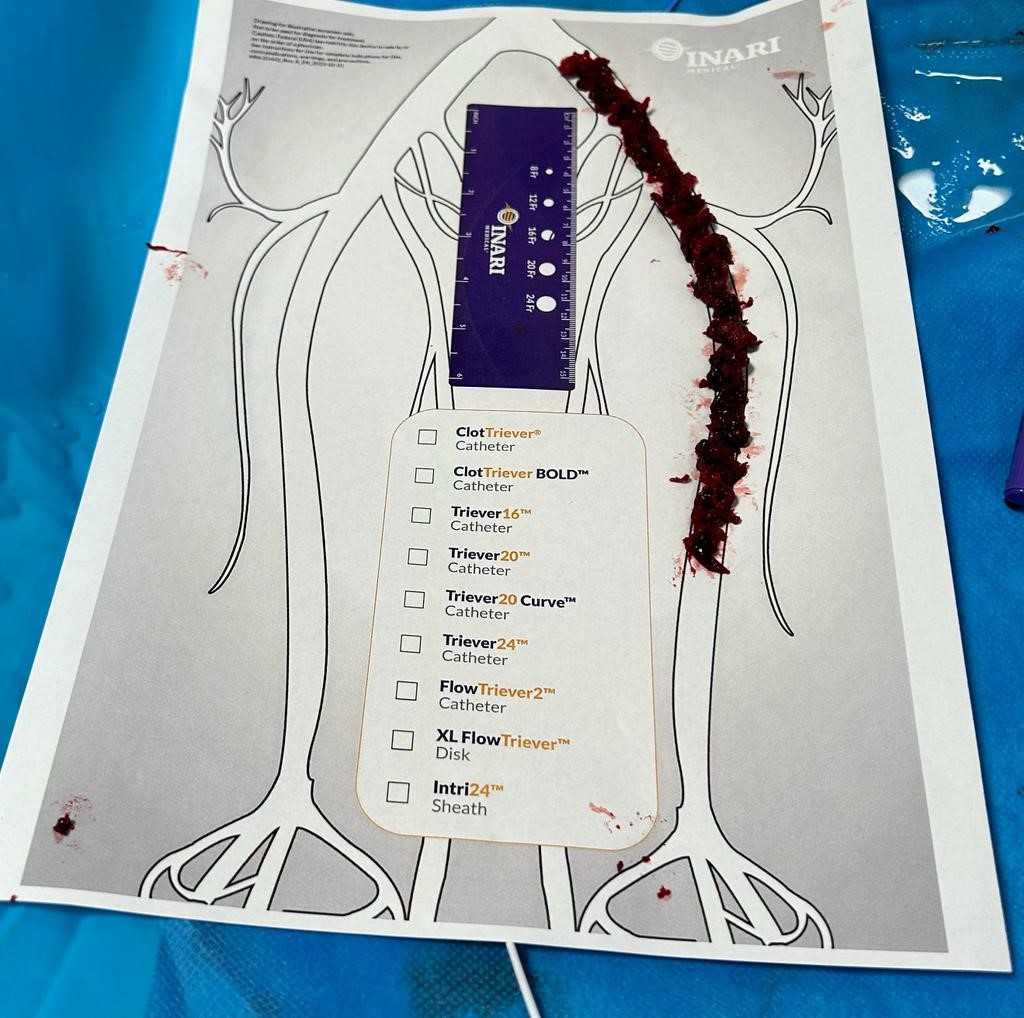
Clot removed with INARI device
“Traditionally, this would have been treated with anticoagulation. So, you would put them on blood thinners and hope the clots will dissolve, or we would use a more potent clot busting agent call lytics to dissolve the clots. The problem with lytics is, because you’re using a medication that is dissolving the clots, it also makes your blood thin, meaning a risk of bleeding,” said Dr Lim.
Dr Lim explained that patients who need lytic therapy will need to spend some time in ICU. This is due to them having to be monitored in case they develop a bleeding in the brain, which could be catastrophic.
“They’ll probably be the most stable patient in ICU, and they can be in there for up two or three days. Using this new device means the risk of bleeding elsewhere in the brain and body will be almost zero and they’ll be discharged tomorrow, freeing up a valuable bed in ICU,” says Dr Lim.

Shueh Hao Lim, interventional radiologist and Jaison Abraham, intervention radiology nurse.
Dr Lim described the device as like a ‘fishing trawler’, explaining, “once it’s deployed, we put the ‘big net’ into the healthy section of the vein and you pull back. It starts to pull out all of the clots”. The ‘net’ is 15-20cm long, with the whole device being longer so it can come up the leg.
He was assisted during the procedure by vascular surgeon, Melvinder Basra, intervention radiology nurses, Linda He, Jaison Abraham and Anna Belependio, medical radiation technologist, Bronwyn Chapman and anaethesist, Victoria Lyon.
The team: From L-R Shueh Hao Lim, interventional radiologist; Linda He, IR nurse; Bronwyn Chapman, MRT; Jaison Abraham, IR nurse; Anna Belependio, IR nurse. Other people not in picture - Victoria Lyon, anaesthetist and Melvinder Basra, vascular surgeon.
An anaesthetist was needed in this procedure because the patient had developed May-Thurner syndrome, a condition that results in the iliac vein being compressed. Common symptoms are swelling of the legs and ankles, pain, tingling, and/or numbness in the legs and feet.
Dr Lim met with the patient the day after the procedure, and they commented on how their symptoms had completely vanished.
“The leg swelling and pain significantly improved. And suddenly the blood starts to flow back in”
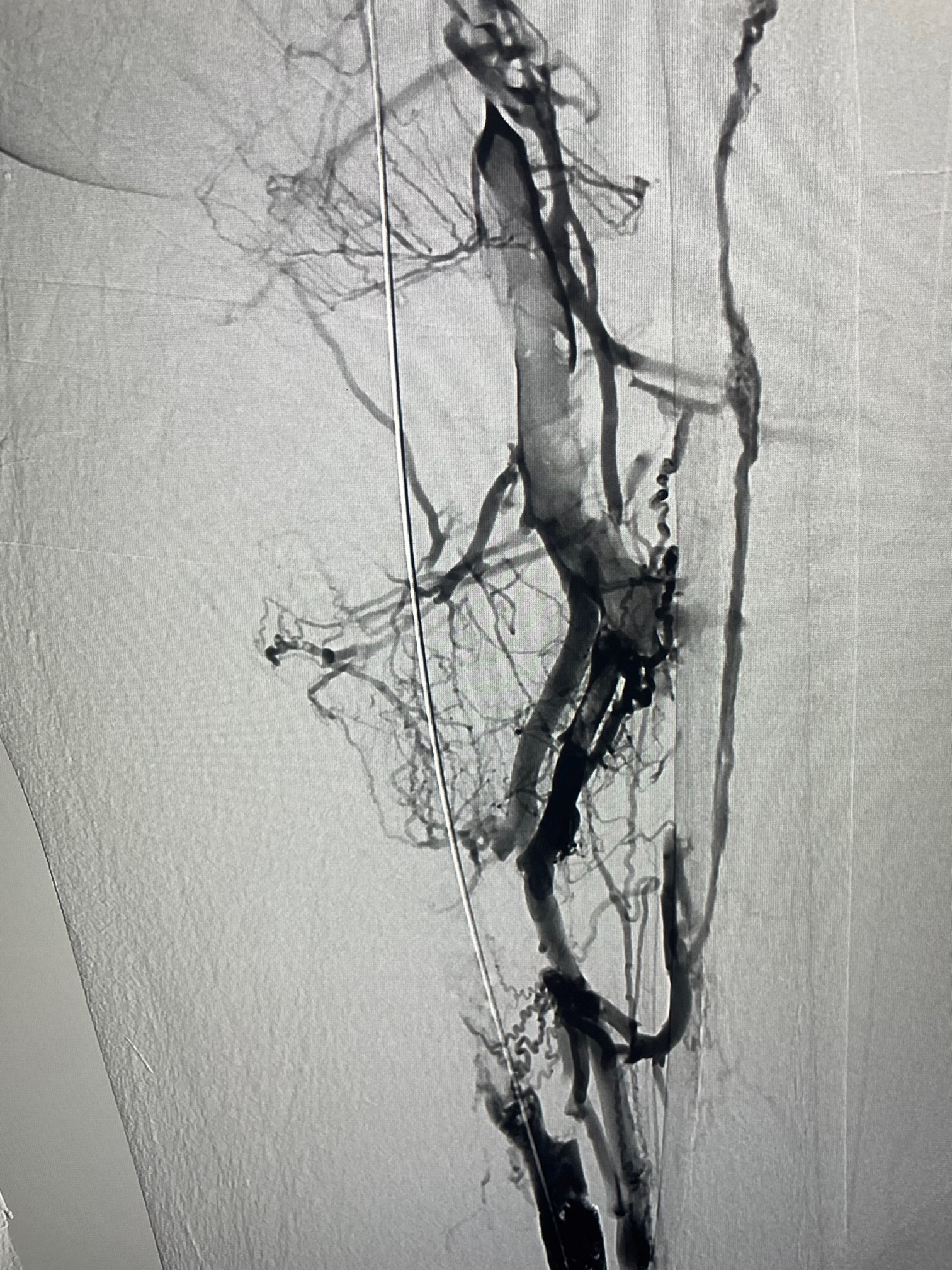

Picture of clot before and after the procedure
Dr Lim and his team at Wellington Regional Hospital continue to explore and implement cutting-edge technology, offering patients innovative solutions and a brighter outlook for their medical conditions. With these advancements in interventional radiology, patients can look forward to shorter hospital stays, quicker recoveries, and improved quality of life.